Last week, the Care Quality Commission (CQC) published a devastating report into the Youth service based at 80 St Stephen’s in Norwich, which is supposed to support young people in Norwich, North Norfolk and South Norfolk.
It is the worst report we have ever read, even by the appallingly low standards of Norfolk & Suffolk NHS Foundation Trust (NSFT), the worst mental health trust in the country.
We are told that the first day of the inspection was so bad that staff feared the service would be closed down and believe they only survived because there was nowhere else to send young people in Norfolk or Suffolk. There is no more powerful case for the breaking up of the monopoly of NSFT.
We carried out this inspection of 80 St Stephens Road, Norwich Youth team, as a result of whistleblowing information and other intelligence. This was a focussed, responsive, unannounced inspection specifically to look at patient case management, staffing and team management/leadership.
The unannounced inspection took place after senior clinicians whistleblew to CQC. Front line staff trying to do their best have endured underfunding and self-serving, incompetent, nepotistic management for far too long.
Incredibly, the CQC report raising safety concerns has not, at the time of writing, been shared with front line clinical staff, NSFT’s governors or other stakeholders, despite CQC publishing the report on its website last week and the trust’s management receiving the report weeks ago.
This CQC report is far from the first inspection report to find that NSFT’s mental health services for Children, Families and Young People (CFYP) are inadequate.
The Service Director, Rob Mack, is not a new appointment to CFYP or NSFT. Rob Mack has been in charge for over two years and was previously the deputy in charge.
At the time of the radical redesign at NSFT, during which mental health services were cut or closed, staff were made redundant or downbanded, average staff salaries fell substantially in absolute as well as real terms and the number of unexpected deaths doubled, Rob Mack was a Band 8a (salary of up to £46,621 in 2012/13).
Three years ago, Rob Mack became the Deputy Director of CFYP. Six months later, in March 2018, his boss, Andy Goff, left NSFT and Rob Mack took charge of CFYP and he was put on Band 8c (salary of up to £71,243 in 2018/19).
Last year, for reasons unknown, Rob Mack’s salary band increased again to Band 8d (salary of up to £87,754 in 2020/21).
So, as mental health services for Children, Families and Young People have failed, Rob Mack’s pay has increased by around 88 per cent. That’s nearly doubled.
During the disastrous radical restructure, Rob Mack was involved in organising the candidate interviews at Carrow Road. In the radical restructure, Rob Mack’s brother, Andy Mack, was also coincidentally appointed to a Band 8d job at NSFT (salary of up to £87,754 in 2020/21). Rob Mack secured his continuation in his job as CFYP Service Director in the new structure without competitive interview shortly thereafter.
The radical restructure also saw the re-employment of Amy Eagle, who had helped destroy adult mental health services which were then based at 80 St Stephen’s, as an additional layer of bureaucracy on a doubled salary, as Deputy Chief Operating Officer and Rob Mack and Andy Mack’s boss. Amy Eagle is coincidentally best friends with the Head of HR at NSFT, Sarah Goldie. The only candidate interviewed for the post of Deputy Chief Operating Officer of NSFT, other than Amy Eagle, was Rob Mack’s brother, Andy Mack.
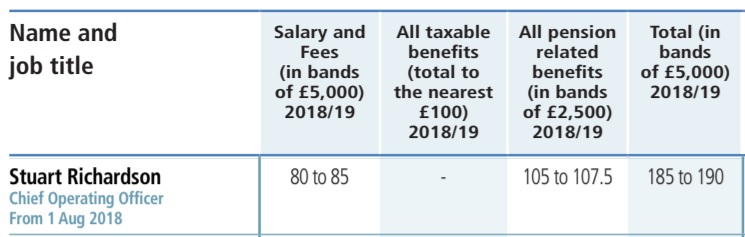
£90k+ Amy Eagle reports to NSFT’s Chief Operating Officer, Stuart Richardson, who, according to NSFT’s Annual Report and Accounts 2018-19, trousered total remuneration of £185,000 to £195,000 from NHS coffers in just eight months in the job in 2018-19, as mental health services went into meltdown. Here’s the section of the Annual Report, as otherwise it will be denied:
Front line clinicians have repeatedly told us that NSFT will not improve until managers and directors are held accountable for their actions and decisions.
Managers at NSFT believe they are entitled to vast pay rises but should take no responsibility for performance.
Marie Gabriel, NSFT’s Chair, promised us she would not tolerate underperformance by managers.
Board directors at NSFT need to read this inspection report and explain to service users, carers and front line staff why Rob Mack is still employed by NSFT.
There are many more important questions for NSFT to answer which we will pose in the next few days.
The people of Norfolk and Suffolk have been let down for far too long.
Too many people have paid with their lives.
It isn’t just mental health services that are Inadequate: it is NSFT’s senior management and Board.
This is what CQC discovered at 80 Stephen’s during its unannounced inspection:

The team lacked effective systems to monitor and manage referrals, triage, assessment and treatment. None of the staff we spoke with understood the process or even knew if there was a process. This meant it was impossible to be assured that systems were safe and patients were seen in a timely and effective way.
Staff were concerned that there was an expectation to address the waiting list for assessment without the resource in place to then offer any treatment identified in this process.
There was a disconnect between the clinical team staff and managers. We spoke to a team that was fractured, concerned about the management of risk and lacking in leadership. We saw staff moving in different directions, making decisions about their work that did not follow process as there was a lack of understanding of what those processes were. Some staff felt they were not listened to when they tried to raise concerns
During the inspection we heard of a significant number of meetings, some with a lack of structure, clear agenda and process. It was significant that every member of staff spoken with did not understand the meeting structures or have a clear awareness of processes they needed to follow to address issues.
We were not assured that waiting lists were accurate and this was also verified by the team managers.
Patients on those waiting lists were not always being adequately monitored or supported.
Where a change in the patients’ individual risk was identified, their risk assessments were not always being updated.
We also found some appointments and therapy groups being cancelled as there were not enough staff available. This meant that there was a risk that patients whose needs changed might not be identified or receive support in a timely manner.
The building at 80 St Stephens Road was not well maintained and the décor was shabby. Internet access at the time of the inspection was not reliable which meant that patient records were not always accessible.
Staffing had not always been sufficient to meet patient need. In December 2019 there were large gaps in staffing in the North team. There was one Band 7 vacancy, four Band 6 vacancies and one Band 4 vacancy. This meant there were only two Band 6 staff in post in the North team. This was insufficient to address the needs of patients. Evidence of impact was reflected in patients’ records. We saw that patients were not always being seen by clinicians in a timely way and that therapy groups were cancelled on more than one occasion.
There was an increase in patients being added to the team-held waiting lists at this time due to staff leaving and a heavy demand from referrals. Staff admitted they had significant concerns that they could not manage caseloads safely and that patients were not always being seen according to their need or risk.
We reviewed 10 care records and found that four did not reflect all of the patients’ current risks. For instance, it was discussed in a team meeting that a patient’s parent was at risk. This was not documented in the patient’s records. Crisis plans, if in place, were minimal in content, often just listing phone numbers of who to contact and lacked plans specific to the individual.
We were not assured that processes for managing waiting lists, particularly team-held waiting lists, kept people safe. Where a patients’ risk was discussed in team meetings and there was an identified change to risk, we saw that risk assessments were not always updated. There was no clear process to ensure patients on team-held waiting lists were appropriately monitored and supported. We saw large gaps in records, with one patient not having had direct contact since July 2019. Patient waiting list concerns had been mentioned at the last four inspections and it was disappointing that this had not been fully addressed within this team.
Discussions about patients at case meetings did not always translate into action and did not transfer into patient records. It was unclear how actions were implemented and who was responsible to follow them up. Staff confirmed this was a risk.
The building at 80 St Stephens Road was not well maintained. The décor was shabby and internet access was not reliable. The unreliable access to the internet meant that patient records were not always accessible. We saw this during inspection when there was a lack of access for several hours. Consequently, some patient sessions were cancelled by one of the teams in the building.
The business resilience plan for the trust lacked sufficient detail at a local level. The plan talked about such events as loss of access to clinical records, however, there were no locally driven protocols to manage such events. This is despite it being a known issue as loss of connectivity had happened on previous occasions.
There was a lack of structure for discussing lessons learned at meetings. Local team meetings did not have a clear meeting agenda. We saw that few meetings were documented as actually taking place although we were told some were happening. Of those meetings that did take place, there were several where lessons learned were not discussed at team level, despite there being discussions at clinical governance meetings.
There was no clear process to ensure patients on teamheld waiting lists were appropriately monitored and supported. We saw gaps in records; one patient had not been contacted since July 2019. Another patient had
several attendances at the acute hospital emergency department whilst waiting for allocation, the GP had followed up with concerns and in the summer of 2019 the liaison staff at the Accident and Emergency department submitted an incident report due to the lack of availability for support from the youth team.
A further patient had been referred to the team in March 2019. The patient was added to the waiting list for a care co-ordinator in July 2019 but only made it to the priority meeting in January 2020. We were not assured that processes for managing waiting lists, particularly team-held waiting lists, kept people safe.
We reviewed the early learning report from a recent serious incident. We saw that at the time of the incident, the patient had recently been seen by clinicians. However, in the months prior to this we saw missed opportunities to engage with the patient, cancelled appointments and
cancelled group sessions due to staff sickness. We saw evidence of a decline in the patients mental health that was not immediately acted upon. The patient was on the teamheld list and did not have one single clinician overseeing their care. This is currently subject to a full root cause analysis investigation that has not yet been completed.
There was a lack of structure for feeding back lessons learned at meetings or via other methods of communication. Local team meetings did not have a clear meeting agenda and we saw that few meetings were documented as actually taking place. Of those meetings that did take place, there were several where lessons learned were not discussed at team level, despite there being discussions at clinical governance meetings.
The clinical lead showed us evidence of 54 patients on the North ‘team-held’ waiting list. The longest time a patient had been waiting was over 12 months. Plans were in development to address this as a priority action.
The lead nurse provided data that showed there were a total of 228 patients waiting for assessment, 149 of which were outside of the target for assessment.
The team was fractured and concerned about the management of risk, lack of leadership, clear structures and processes. We saw staff moving in different directions, making decisions that did not follow process as there was a lack of understanding of what those processes were. Some staff told us that there was an air of learned helplessness and acceptance that the team was not functioning as it should.
Several staff expressed concern that the lack of structure hindered their ability to carry out safe and effective care and that they did not feel listened to when raising concerns. There was a disconnect between the team and managers.
We were not assured of the governance structures within the team at 80 St Stephens Road. We saw a high number of meetings, with a lack of structure and process. It was significant that every member of staff spoken with did not understand the structures or have a clear awareness of processes they needed to follow. We were told of different structures from different staff.
We were not assured of processes to manage events such as loss of power and how the service would minimise risk to patients. However, we saw some work had commenced to look at this. Managers gave us a draft business impact analysis spreadsheet showing identified risks of not being able to deliver services. The business continuity plan or resilience plan provided oversight on what needed to happen in certain events such as loss of power. The team were unaware of there being any local protocols or plans on how this would be implemented within the local team.
During inspection when there was a loss of access to the clinical records, one clinician told us that they planned to cancel appointments as it was unsafe. There was no thought to contact other services to access the information or consider an alternative plan.

This report and comments by the Campaign to Save Mental Health in Norfolk and Suffolk does not surprise me. What shocks me is that the situation at NSFT, which appears to be led by self-serving, inefficient, hubristic, dishonest people, is allowed to continue. The people and organisations, including CQC, the Non-executive Directors and governors of NSFT, NHS England, and the government, including our local MP – the Minister of Health have not succeeded in weeding out and exposing poor, disastrous management at NSFT and its current effects on local mental health services. No representative of the Trust appeared brave or professional enough to appear for comment on local BBC news. Where is the CEO and the Chair? I remain disgusted, dismayed and very angry with the continuing situation with services provided by NSFT.
Obscene salaries
I am a website designer. Recently, I am designing a website template about gate.io. The boss’s requirements are very strange, which makes me very difficult. I have consulted many websites, and later I discovered your blog, which is the style I hope to need. thank you very much. Would you allow me to use your blog style as a reference? thank you!
Howdy! Quick question that’s completely offf topic.
Do yyou know how to make youjr ssite mobile friendly? My blog loopks weiird wwhen browsing from mmy iphone4.
I’m tying to find a templatre or plugin that might be able
to resoove this issue. If yoou have anny recommendations,
please share. With thanks!
Excellent wway of explaining, andd good paragraph too ttake data
concerning mmy presentatioon subject matter, which i am going
to deliver in college.
I really like your writing style, good information, thankyou for putting up : D.
My spouse and I stumbled over here different website and thought I
may as well check things out. I like what I see so now i am following
you. Look forward to looking at your web page yet again.
Here is my web blog vpn special code
I blog often and I truly thank you for your content.
This article has really peaked my interest. I’m going to
bookmark your site and keep checking for new details about once a week.
I subscribed to your RSS feed as well.
My web page – vpn special coupon code 2024
It’s actually a cool and useful piece of info. I am happy that you
just shared this helpful info with us. Please stay us informed like this.
Thanks for sharing.
Feel free to visit my blog post vpn code 2024
Great article! We are linking to this great article on our website.
Keep up the good writing.
Look at my blog :: vpn special code
Hi friends, fastidious paragraph and nice arguments commented here,
I am actually enjoying by these.
Also visit my webpage vpn coupon 2024
Excellent goods from you, man. I’ve take into accout your stuff
prior to and you are simply too fantastic. I really like what you have got here, certainly like what you are saying and the best way by which you are saying
it. You are making it entertaining and you continue to care for
to keep it sensible. I cant wait to learn much more from
you. This is actually a terrific web site.
my website: vpn special coupon code 2024
Hello to all, as I am in fact eager of reading this webpage’s post to be updated on a regular basis.
It contains fastidious data.
Here is my webpage – vpn 2024
Everything is very open with a very clear description of the issues.
It was definitely informative. Your site is extremely helpful.
Thank you for sharing!
Feel free to surf to my page – vpn 2024
I’ve been surfing on-line greater than 3 hours lately, yet I never found any fascinating article like yours.
It’s beautiful price sufficient for me. In my view, if all
web owners and bloggers made excellent content material as you
probably did, the internet can be a lot more helpful than ever before.
Here is my webpage … vpn coupon code 2024
hello there and thank you for your info – I’ve certainly picked up something new from right here.
I did however expertise some technical points using this site, since I experienced to reload the site a lot of times previous to I could get it to load correctly.
I had been wondering if your hosting is OK? Not that I am complaining, but slow loading instances times
will sometimes affect your placement in google and
could damage your quality score if advertising and marketing with Adwords.
Anyway I’m adding this RSS to my email and could look out for much more of your respective interesting
content. Ensure that you update this again very soon.
Have a look at my site :: vpn special
How Does Sugar Defender Work & What are the Expected Results? Sugar Defender is a liquid supplement.
I would like to thnkx for the efforts you have put in writing this web site. I am hoping the same high-grade site post from you in the upcoming also. Actually your creative writing abilities has inspired me to get my own web site now. Actually the blogging is spreading its wings quickly. Your write up is a great example of it.