The original pdf version can be downloaded here.
A contribution to Norfolk County Council’s Health Overview & Scrutiny Committee from the Campaign to save Mental Health Services in Norfolk & Suffolk
January 2014
“Worldly wisdom teaches that it is better for reputation to fail conventionally than to succeed unconventionally”
John Maynard Keynes, The General Theory of Employment, Interest and Money
“Tout est pour le mieux dans le meilleur des mondes”
Dr. Pangloss in Voltaire, Candide
Who are we?
We are a cross-party campaign started by front line staff, people who use NHS mental health services, carers, families and concerned members of the public in Norfolk and Suffolk to fight against the cuts and ‘radical redesign’ at Norfolk & Suffolk NHS Foundation Trust (NSFT). Many members of staff, service users and carers are actively involved in the Campaign which agreed its priorities at a public meeting attended by hundreds of staff and service users, which saw many more turned away for lack of space. The Campaign has more than 1,250 supporters. The Campaign isn’t following any political agenda – it has members from across the political spectrum – and will resist any attempt to portray it as partisan. Our campaign has been featured on the BBC News website, on BBC Radio Norfolk and BBC Radio Suffolk, in the EDP, EADT and many other local newspapers. Since its creation less than a month ago, the Campaign’s website has had more than 4,500 visits and the Campaign’s Facebook has a weekly reach of more than 3,000 people.
What do we believe?
We want to see a successful provider of mental health services based in Norfolk & Suffolk, providing skilled employment in the east of England and excellent services in Norfolk, Suffolk and perhaps beyond. However, despite its rhetoric, the current trajectory of NSFT gives little confidence that this will be achieved. The Campaign opposes the historic underfunding of mental health and the NSFT Board’s collaboration with unduly-harsh funding cuts, its wasteful and ill-thought out reorganisations and its disproportionate slashing of front-line services to the most needy and vulnerable.
What do we propose?
We have released an Open Letter to the Board, with a practical six-point plan, the implementation of which will begin to restore confidence in mental health services. This Open Letter is included at the end of this submission. The Campaign believes that the NSFT Board should change course or resign as there is no time for delay. The Campaign also strongly believes that commissioners must recognise that the level of bed and community provision in Norfolk and Suffolk is deeply inadequate and that planned cuts cannot possibly go ahead until it is demonstrated that the provision is not required, which is far from being the case today. We provide further information and recommendations in this paper.
Why are we submitting this paper to HOSC?
The Francis Report highlighted the importance of NHS bodies listening to patients, carers and staff and the importance of the role of local government in holding the NHS to account. We believe that the excellent report produced by the now-disbanded Joint Norfolk & Suffolk committee has been the only serious and transparent investigation into the ‘radical redesign’ and we wish to support the work of the Committee by providing an alternative narrative to that put forward by NSFT. Only since we began campaigning have some of the NSFT Board acknowledged there is a ‘developing crisis’ in mental health services – before that the NSFT Board denied that cuts to services were taking place – only ‘improvements’ in the Panglossian world of the ‘radical redesign’. Sadly, it appears that there is no local mechanism for the removal of an NHS Trust Board, despite the expense of the recruitment of Foundation Trust members and governors, which to us seems extraordinary. The only body with the power to intervene is Monitor, which has competition rather than quality of care as its primary focus and is a national and unelected quango rather than a local and democratically accountable body.
Since NSFT introduced the ‘radical redesign’, NSFT has lost its Chief Executive and doesn’t have a replacement. The Chair of the Trust has retired, as has the Director of Nursing. Laurence Mynors-Wallis, the Registrar of the Royal College of Psychiatrists and himself an NHS Medical Director, has said that consultant psychiatrists in Norfolk and Suffolk have serious concerns about the impact of the ‘radical redesign’ at NSFT on patient safety. The Royal College of Psychiatrists took the unprecedented step of writing to health regulator, the Care Quality Commission (CQC). NSFT is a rudderless organisation which continues to ignore the opinions of the majority of its clinicians and desperately needs HOSC’s help to point it back in the right direction. We believe that NSFT was given the benefit of the doubt by Scrutiny rather than wholehearted supported in its last report but now there is a great deal more evidence about the disastrous results of the implementation of the radical redesign.
What is wrong with the ‘radical redesign?’
At the heart of the ‘radical redesign’ are two key elements: the supposedly innovative Access & Assessment Teams (AAT) and a reduction in the need for beds through improved services in the community. We will look at each element in turn and then ask ‘Where has the money gone?’
Access & Assessment Teams
Why were AATs established?
The AAT model has been presented as an innovative improvement but the main initial reason for its attractiveness to NSFT was its anticipation of the introduction of Payment by Results (PBR). AAT was established in February 2013 in anticipation of PBR being introduced in April 2013, even though its likely delay or cancellation had been widely signalled in the press. The introduction of PBR for mental health has since been delayed for at least two years and it is now very unlikely that it will ever be introduced in the anticipated form. The primary purpose of AAT was to offer a single point of access for all referrals to allow them to be put into charging ‘Clusters’ thus allowing the capture of all chargeable ‘customers’ with accurate data for invoicing purposes. Given the centrality of PBR to the radical redesign model, many within NSFT still refuse to accept, even given Norman Lamb’s public announcement that PBR wasn’t suitable for mental health, that PBR is not going to happen any time soon and bemoan the block contract model. However, it is naïve to believe that commissioners were suddenly going to find considerable additional funding for mental health solely on the basis of a change in funding model.
What did AAT replace?
In central Norfolk, AAT it replaced the primary care mental health teams, which consisted of link workers attached to GP surgeries and three dedicated consultant psychiatrists who provided clinical support to GPs. Link workers were extremely popular with GPs and patients. The AAT models are different in different parts of NSFT but this paper, for the sake of simplicity, is restricting itself to the model in central Norfolk.
What has gone wrong with AAT?
Underestimated number of referrals
The anticipated number of referrals into the service was markedly underestimated, possibly because much of the work previously done by link workers (advising GPs on cases) was never recorded or understood by NSFT. The anticipated number of referrals for Central and West Norfolk was between eighty and ninety per day but the actual number is around 120 per day. We do not have the exact current numbers but we are confident that they are reasonably accurate and NSFT can supply the recorded numbers to the committee.
Inadequate resources
AAT was inadequately resourced according to these anticipated underestimates and, to make matters worse, has had significant problems with sickness and so has never been adequately staffed to manage the number of referrals it receives. This is the case for services in both Norfolk and Suffolk.
Failure to hit performance targets
AAT Norfolk has never been able to keep to its emergency (4-hour), urgent (72-hour) or routine (28 days) targets. This autumn, we believe that 72-hour referrals were taking about a fortnight to be dealt with and 28-day referrals were taking about two months. The Campaign has submitted a Freedom of Information request to NSFT (FOI 01, 2014), which the Campaign will share with the Committee once it receives a reply, but the figures leaked to the press previously are as follows: only 52 per cent of emergency referrals were dealt with within four hours; only 32 per cent of urgent referrals were dealt with within 72-hours and only 33 per cent of routine referrals were dealt with within 28 days. The Operations Director of NSFT has claimed that NSFT’s own figures are ‘wildly inaccurate’ but has typically not supplied any more accurate ones. Multiple supporters of the Campaign with knowledge of the performance of AAT agree that the leaked figures are misleading – they believe the situation is actually worse.
Unpopularity with GPs
NSFT claim that GPs are happy with single point of access but there have been a very large number of complaints by GPs about AAT and lots of negative feedback. Many GPs say that they much preferred the previous link worker service.
Why is AAT delaying treatment and adding cost?
To fully understand the impact of AAT, the system for receiving, processing and assessing referrals needs to be outlined: 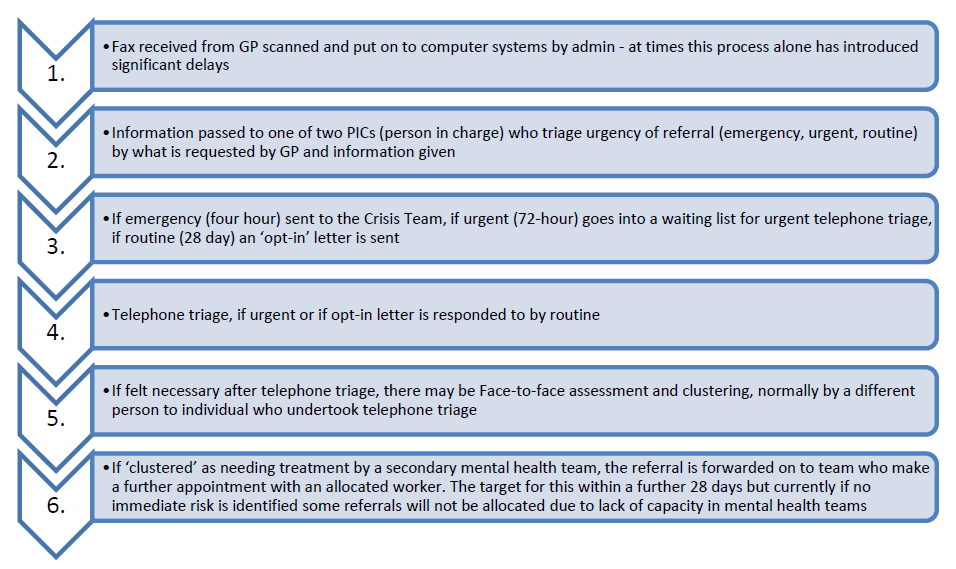 This complicated and expensive system introduces long delays before the receipt of treatment, if the referral is even allocated at the end of the process. Distressed patients have to repeat their stories to three different individuals, one of whom they never see and another they will never see again.
This complicated and expensive system introduces long delays before the receipt of treatment, if the referral is even allocated at the end of the process. Distressed patients have to repeat their stories to three different individuals, one of whom they never see and another they will never see again.
Devastated staff morale
AAT has lost its original manager, both of its initial consultant psychiatrists and many other staff, including clinical team leadership, in less than a year. Staff morale has gone from buoyant as part of a new, flagship service to incredibly low and there have been meeting with unions about concerns about an unsafe working environment and practices, lack of resources and lack of support from senior managers. Staff report very low job satisfaction and feeling that they are unable to do any good for the people they see because of time pressure and lack of resources and ongoing input into their care. They have described it as like working in a sausage factory or like being a battery chicken but not producing eggs. NSFT claimed that AAT would be wonderful because staff had received call centre and customer care training but failed to realise that making skilled and high-risk psychiatric assessments on the phone is a very much more demanding task than reading a bank balance on a computer screen, taking an order for a new broadband service or setting up a direct debit at a utility firm.
Consequences of the failure of AAT & Recommendations
AAT was trumpeted as a single point of contact but has become a single point of failure. Nearly all clinicians and operational managers, privately at least, believe that AAT is the wrong model but the Board stubbornly and damagingly refuses to acknowledge that, at the heart of the radical redesign, AAT was and remains a terrible mistake, and continues to throw money it does not have at the problem. AAT is a money pit without purpose at the centre of the Trust Service Strategy. The highly skilled but demotivated staff in AAT should be reallocated into the community where they can treat people rather than delay treatment assigning referrals to accounting codes which will most likely never be used.
Reduction in the need for beds through improved services in the community
There is a bed crisis
NSFT claims that it has sufficient beds and criticised this Campaign for calling the current scenario a crisis. However, the number of transfers of acute adult or psychiatric intensive care patients to third party providers, frequently many miles away from home, is growing at an extraordinary rate for a service with sufficient capacity. The main defence of NSFT to accusations that it does not have enough beds seems to be to say that there aren’t enough beds in the entire country. Similarly, when presented with a clear case of suicide immediately after a promised voluntary-admission bed was unavailable, the Trust resorts to statistical analysis and commissioning a report by a member of its own Board to deny an obvious truth. This tendency to seek corporate solace in statistics and denial has worrying similarities to what the Strategic Health Authority did when faced with Mid-Staffs complaints and mortality data.
The number of crisis patients who could not be accommodated by NSFT was relatively low and stable before the ‘radical redesign’, occurring once every couple of months (seven in the financial year 2010/11 and six in the year 2011/12). However, in 2012/13 the number of patients who could not be found beds grew by 750% to 51. In the first six months of this year, 33 patients in crisis could not be found a bed, a further increase of 27.2%, which represents a 1000% increase in the number of seriously ill crisis patients who cannot be found beds since 2011/12. These figures can be readily confirmed (FOI 171, 2013).
There is a very high financial and human cost
The cost of these placements in out of area beds is many millions of pounds. There is a high human price as service users find themselves many miles away from their families and friends. NSFT has stated that it will not help service users families with the cost of visiting relatives placed many miles away through no fault of their own: ‘It is however worth noting that under the NHS Help with Travel Costs Scheme (HTCS) visitors to hospital are not entitled to claim for costs of visiting.’ (FOI 224, 2013). The Campaign has highlighted a recent CQC report which detailed how a husband had run up bills of £3,000 visiting his wife after the closure of dementia beds in King’s Lynn and how he had been misled by NSFT that his travelling expenses would be met (available on our website).
Lack of beds is preventing treatment and putting pressure on overstretched community teams
The lack of beds also places an additional strain on community teams and is in combination with the cuts to community teams is preventing some of the most poorly and vulnerable service users from starting or restarting Clozapine, the NICE recommended last resort treatment for psychosis. The Campaign has highlighted this issue, a Clozapine Crisis, in its 12 Days of Christmas Campaign.
The very community teams who are supposed to keep patients out of hospital have been slashed to breaking point
For the sake of brevity, we restrict consideration here to the two largest teams, which now cover central Norfolk and Norwich, the new North and South Central community teams.
These teams replace three previous localities: North Norfolk, South Norfolk and Norwich City, and saw the abandonment of specialist teams providing assertive outreach (for chronically psychotic difficult-to-engage patients) and brief intervention, homeless and recovery teams. The two new teams have additionally taken over much of the work previously undertaken by link workers. Staff who provided services in Norwich have been removed from their highly productive location at 80 St Stephen’s , leaving no base in Norwich for staff and no dedicated space to see patients for the south central team, i.e. more than half of Norwich and south Norfolk. Gateway House, a rented office building located on a business park in Wymondham, has no facilities to see service users and proposals to provide clinical space have been rejected by the NSFT Operations Director. This relocation and lack of clinical space has had a devastating effect on productivity, with travelling times greatly increased and face-to-face time with patients decreased. The loss of the assertive outreach team is a major problem because without this assertive approach many service users disengage from treatment and become unwell – requiring long and expensive periods in hospital after posing a significant risk either to themselves, or occasionally, others.
Many consultant psychiatrists only discovered what was proposed by the ‘radical redesign’ when it was announced. Those who have raised clinical concerns have been accused of ‘shroud waving’. Consultant psychiatrists do not have job descriptions. NSFT has tried to explain this treatment of its most senior clinical leadership with the excuse that the new positions after the current reorganisation are only ‘temporary’ and that consultants continue to do their old existing jobs, which they clearly do not, until April 2014, when there will be yet another expensive and disruptive reorganisation and it is proposed that there will be cuts in the number of doctors. As we understand it, NSFT still proposes to slash the number of consultant psychiatrists it employs, from about 100 to 67, when the transitional funding provided by the CCGs runs out. The Campaign fails to understand how this, particularly given the large number of locum doctors currently employed by NSFT and which it appears are needed to deliver a decent service, will not have a catastrophic effect on the delivery of services.
Caseloads of band five and six staff are already above recommended limits, the majority hovering around forty but with some higher still. In the absence of link workers and psychiatrists preventing referrals in primary care by dealing with issues in GPs surgeries, there are unsustainably high numbers of weekly referrals to the two new teams – in the region of 30-40 across both teams. These new referrals are targeted to be allocated to the teams and seen within 28 days but this is proving impossible with existing resources, so in some cases only those deemed at risk have been allocated and the rest are placed on an ever-extending waiting list, adding to the 130 cases unallocated since the creation of the teams. It is very difficult see how this number will not just continue to increase for, while a few extra staff have been recruited, the situation will become much worse in March 2013 when between a quarter and a third of existing staff will leave through NSFT’s poorly planned, poorly implemented and hugely expensive voluntary redundancy scheme.
The loss of compassionate support for people with mental illness
Mental illness is frequently precipitated by, and almost invariably leads to, great emotional distress and suffering. None of us need to be told what it is like to suffer, as distress and suffering are sadly an unavoidable part of the human condition. For people with mental illness this distress can be very deep, profound and of long duration.
When distressed we commonly find relief in our friends and family. Talking about what grieves us, with someone who cares for us, can help us find comfort and maybe enable us to put our problems in better perspective, allowing us to begin to see a way through our confusion.
Mental illness leads to great social isolation for many, and, even when friends and family desperately want to help, the nature of the sufferer’s symptoms can frequently make it very hard to understand the best way to do so, leaving those who love the sufferer also in great distress and desperate for help.
Mental health professionals have the capacity to provide great comfort to people with mental illness in their distress. Many service users can testify that having someone with the skills and experience to just listen to their frightening and distressing experiences, without fear or judgment, has helped them to see a way though desperate times. This help often prevents the escalation of issues and the expense of hospital admission or the further involvement of mental health and social services or sometimes the justice system and the Coroner’s Court.
However, for this to be possible there needs to be an ongoing relationship of trust, not a single forty-five minute or one hour appointment with an “assessor” from AAT, or a series of delayed conversations with different people from a community team because of frequent reorganisations. The best outcomes follow from the continuity of care rather than the increasingly all too frequent situation of being placed on an “unallocated” list and told to phone in to speak to whoever is “on duty” if they feel distressed.
Providing compassionate support for people with mental illness in distress is not an emotionally easy thing to do. We all know how draining and demanding listening to friends and relatives in distress can be, and how this can become irritating and annoying if we too are upset, busy or tired. For mental health professionals to be able to offer compassionate support to the distressed it requires them to have the necessary time and emotional space. They need to feel supported and valued by their senior colleagues and this recognition is a vital component of their working environment.
Sadly, many of the staff of NSFT are themselves developing mental ill health through the distress the current situation has placed them in. Many say they no longer feel able to feel sufficient compassion for others because of their own distress, and do not have the time to just listen to service users or have been told that this is no longer what they should be spending time doing: many are either off sick or leaving mental health services as a result.
Having a professional to compassionately listen is vital to the recovery of people suffering from mental illness. It is not a luxury but an essential part of care. Drugs, care plans, and risk assessments cannot heal in the absence of a supportive and caring relationship. There is well recognised, and long known, evidence that one of the most significant factors in reducing the risk of suicide in people with mental illness is the quality of the relationship between the service user and the professionals involved. The provision of a consistent, compassionate, supportive relationship for the treatment of mental illness is akin to the provision of food and clean bed sheets for the treatment of physical illness and the failure to provide it should be taken no less seriously. Unfortunately, and contrary to the clinical evidence, continuity of care and compassion do not feature in the ‘radical redesign’ of NSFT’s services.
Where has the money gone?
Introduction
Like all NHS Trusts, NSFT is expected to make savings of twenty per cent over four years as part of the ‘Nicholson Challenge.’ It is a ‘challenge’ because the savings are supposed to be found through the elimination of waste rather than any reduction in the extent or quality of services delivered. NSFT is not in a unique position.
A high risk approach
For reasons that we do not understand, NSFT rejected the continuous improvement approach, locally and clinically devolved, as has been successfully applied to enhance productivity in too many ‘production’ environments to mention, in favour of a grandiose and rigid four-year plan, which has little focus on productivity or quality, imposed from above, the majority of elements implemented in an accelerated programme within the first two years. This, to us, seems more akin to the industrial planning of Chairman Mao or Soviet Russia, and ignores the variability of public funding, given the reality of local and national political spending settlements and the local priorities of seven CCGs and two Counties. An excellent example of this lack of certainty is the new funding in West Norfolk, which means that an expensive and disruptive redundancy programme and reorganisation has been immediately followed by a another reorganisation and a recruitment crisis in the following year.
Most seriously, there was no local pilot of the proposed changes which seems particularly foolhardy in the case of AATs. Nothing similar, in either design or scale, has been trialled elsewhere. NSFT has been an innovative trailblazer but sadly appears to have chosen to fail unconventionally. This type of ‘gun-ho’ approach seems particularly high risk and foolhardy in the delivery of health services. We will never know whether the ‘radical redesign’ is a failed plan to force CCGs to provide further resources to NSFT or a genuine attempt to ensure that NSFT dominated the seven CCGs. The joint scrutiny report was clear that it felt that the tail was wagging the dog as far the relationship between the supplier, NSFT, and the commissioners, the seven CCGs, was concerned. It appears Monitor’s concerns, when it refused to allow the merger of the Norfolk and Suffolk Trusts on the grounds of a local monopoly dominating mental health service provision in the east of England, were sound and should not have been overturned on appeal.
The ‘consultation’
During the ‘consultation’ it was made clear to staff that only ‘positive’ feedback was welcome, which meant that questioning of both the distribution of cuts between administration and frontline services and questioning the safety of the proposals was unwelcome. Similarly, NSFT have said that they welcome ‘positive’ contributions from this Campaign, which appears to mean we should solely blame the CCGs for providing insufficient resources but not address the performance of the NSFT Board or the ‘radical redesign’ model. We reject this approach. NSFT seems to believe it should spend thousands of pounds on glossy brochures and reports (Expenditure over £25,000 on NSFT website), iPads (FOI 82, 2012), bottled water (FOI 82, 2012) and hiring expensive venues such as Newmarket Racecourse or Dunston Hall for management and ‘leadership’ events while lacking the employees to consistently staff wards properly or to provide sufficient beds to those in distress. Management of change at NSFT can be better described as ‘chaos’ as demonstrated by the inability of NSFT to even provide its management structure to salesman’s standard requests (FOIs 54 and 60, 2013).
Declining staff salaries
NSFT’s Annuals Reports tell us that the average salary of NSFT employees fell by 15.2% or £4,040 each from £26,557 to £22,517 between 2011 and 2013. Salaries have not just been static as part of the public sector pay freeze, they have fallen dramatically in real and absolute terms. The Chair of NSFT has recently stated in the media that eighty per cent of NSFT’s costs are wages. Even without service cuts and redundancies, taking this eighty per cent cost assumption on board, salary reductions alone should have achieved more than sixty per cent of the required costs savings (12.16%). This is not a question of greedy public sector employees failing to share in austerity measures. Some low-paid employees, as detailed in our 12 days of Christmas campaign on our website, cannot afford to put petrol in the cars they need for work. Meanwhile the pay of the Board, Executive and its acolytes has either remained stable or risen due to ‘promotions’ or new opportunities from ‘change’ and ‘being commercial’. This is a large factor in the collapse in morale among frontline staff and the dire findings of the NHS Staff Survey.
Declining numbers of nurses
Further, NSFT Annual Reports show the number of NSFT Nursing, Midwidery & Health Visiting employees has decreased from 1,438 in 2011 to 1,324 in 2012 (a decrease of 7.9%) and further still to 1,250 in 2013 (a further decrease from 2012 of 5.6% and a cumulative decrease since 2011 of 13.1% – 188 fewer nursing posts). Thus in Nursing, Midwifery & Health, if we combine the salary and employee reductions, costs savings in the region of 26.3% have been achieved, far in excess of the 20% improvement target.
Declining numbers of Support Staff
Similarly, NSFT Annual Reports show the number of NSFT employees in Healthcare Assistants and Other Support Staff has decreased from 1,066 in 2011 to 970 in 2012 (a decrease of 9%) and further to 823 in 2013 (a further decrease from 2012 of 15.2% and a cumulative decrease since 2011 of 22.8% – 243 fewer healthcare assistant and support staff posts). Thus in Healthcare Assistants and Other Support Staff, if we combine the salary and employee reductions, costs saving in the region of 34.5%, far in excess of the 20% improvement target.
Declining numbers of social care staff
Again, NSFT Annual Reports show the number of NSFT employees in Social Care has decreased from 111 in 2011 to 61 in 2013 – a cumulative decrease since 2011 of 45% – 50 fewer social care posts. Thus in this category, if we combine the salary and employee reductions, cost savings are in the region of 53.3%, far in excess of the 20% improvement target.
NSFT needs to open its books
So given this scale of salary reductions in the wages and number of front-line staff, where has the money gone and why are more bed closures and job losses planned? These are key question for HOSC. Without access to NSFT’s management accounts, we can only provide some answers.
Increased numbers of bureaucrats
Firstly, while shedding front-line staff and closing wards, NSFT Annual Reports show the number of NSFT employees in Administration & Estates has risen from 975 in 2011 to 1,068 in 2012 (an increase of 9.5%) and to 1,084 in 2013 (an increase from 2012 of 1.9% and a cumulative increase since 2011 of 11.2% – 109 additional administrative posts). As mentioned earlier, some spending by central management appears extravagant at a time of brutal cuts in frontline services and deserved investigation. We recommend that HOSC seeks average salary figures from NSFT for the different categories of employees in their Annual Reports. This will allow the discovery of the cost of these additional 109 administrators and to ascertain the distribution of salary changes between frontline staff and the bureaucracy. If the bureaucracy had suffered similar job cuts to the 22.8% inflicted upon Healthcare Assistants and Other Support staff, there would be 753 employees rather than the 1084 listed as employed in the 2013 Annual Report. Even if these administrators were paid only the average 2013 wage of £22,517, this would liberate £7,453,127 per year to be redirected into patient care. It is very difficult to understand why the bureaucracy is growing while services are being slashed. If productivity is defined as the ratio of outputs to inputs, productivity is falling dramatically at NSFT.
Bloated management structure
The bloated management structure is more than a financial burden. Leading clinicians tell us that if they went to all the internal management meetings to which they are invited they would never see any patients, and, indeed, that managers cannot understand the time pressures clinicians are under and, further, recommend that clinicians behave more ‘strategically’ and see less patients if they want to be ‘taken seriously.’ This output is the exact opposite of what should be desired. Meetings are ‘interminable’, frequently lack an evidence-base and rarely make decisions. Further, that so many people attend but say little ensures that collective responsibility means that nobody takes responsibility. Clinicians report that as managers acquire personal assistants and, in some cases, up to three ‘deputies’, consultants and clinical teams lose skilled administrative and clinical staff.
If NSFT wants to make decisions quicker and to genuinely involve clinicians in the decision-making process, it needs far fewer managers than it has at the moment and to involve clinicians who have a vocation and spend more than one half of the working week seeing service users. It is not enough just to say ‘But we invited you to this meeting but you were too busy to attend.’ Since many of these administrative and managerial staff were once clinical staff, this readjustment process can be achieved with minimal human and financial cost by encouraging administrative staff to move back to the frontline and re-banding them in exactly the same way as has happened with frontline staff.
More than £2.5 million spent on locum doctors
Secondly, NSFT, whilst saying it can slash the number of doctors when the transitional funding expires, is spending a very large amount of money on locum doctors. The NSFT Annual Report indicates that the number of temporary medical & dental staff has increased from 32 in 2012 to 81 in 2013 – an increase in locum doctors of 153% – 49 additional locums doctors. Locum doctors, by definition, are not ideal in terms of continuity of care. The table below, from FOI 208, 2013, shows the cost of agency locums doctors in the financial year 2012/13: 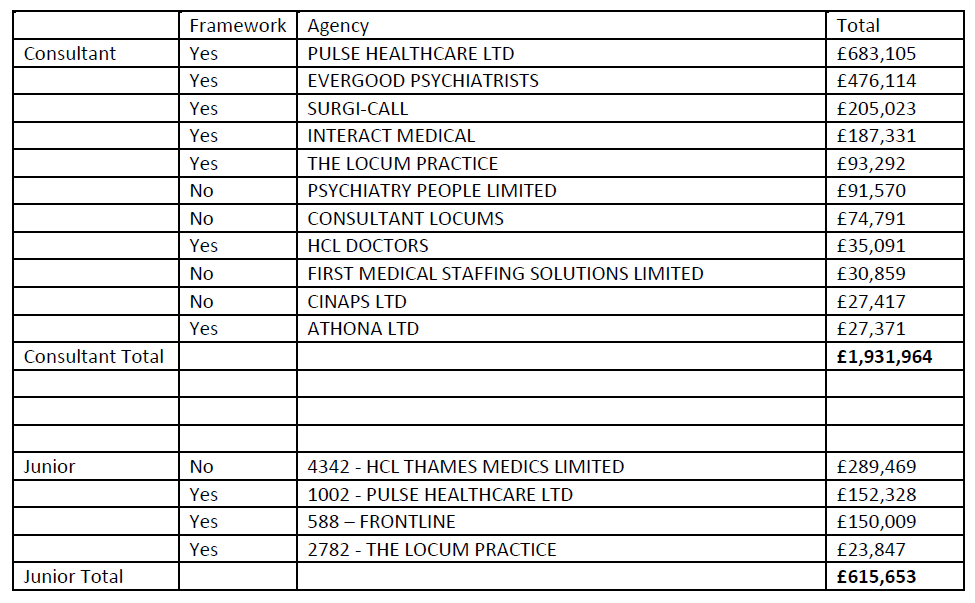 The cost of these temporary medical staff in the 2012/13 financial year was a total of £2,547,617. HOSC needs to seek answers from NSFT about what happens when the transitional arrangements come to an end.
The cost of these temporary medical staff in the 2012/13 financial year was a total of £2,547,617. HOSC needs to seek answers from NSFT about what happens when the transitional arrangements come to an end.
Millions spent on agency and NHSP temporary staff
Thirdly, NSFT is spending large amounts on temporary nursing staff, both agency and through NHS Professionals (NHSP). Expenditure on agency nurses in 2012 was £2,271,426 and on agency Allied Health Professionals was £181,036 (FOI 218, 2103). These figures do not include expenditure with NHS Professionals (NHSP). Based upon the expenditure of over £25,000 data that NSFT has a statutory duty to publish, NSFT spent more than £8 million with NHSP in the most recent twelve month period we analysed (ending July 2013) with a peak expenditure of £1,837,175.61 in December 2012 alone. Yet, despite this scale of expenditure on temporary staff, NSFT appears unable to staff its ward properly:
“The Trust has two Psychiatric Intensive Care Units within its localities. Rollesby Ward based in Norfolk and Lark Ward based in Suffolk. Both wards have ten beds and are mixed sex wards. I confirm that on Rollesby Ward there are 2 nurses on the early and late shift and 1 nurse on the night shift. On Lark Ward they aim as a minimum to have 2 nurses on every shift, supported by 3 support workers, but this is not always achieved.” (FOI 196, 2013).
Low staffing level reports on Norfolk NSFT wards increased from 91 (April 2011-March 2012) to 128 (April 2012-March 2013), an increase of 40.7%. Data for 2013 (only until October 2013) indicates a further increase from 12-13 in the region of 5.8% and our 12 Days of Christmas campaign details worrying concerns expressed by staff in secure services that safe staffing is a serious and urgent problem.
Millions spent on out of area beds and transport
Fourthly, NSFT is spending very significant sums on out of area beds whilst claiming it has excess capacity to cut despite having seven per cent fewer adult beds and twenty nine per cent fewer older age beds than the national average (data from reports of Director of Nursing and Operations Director at last NSFT Board meeting). In Norfolk alone, in 2012/13 NSFT spent £437,000 on out of area NHS beds, £4,866,000 on out of area private beds and £29,000 on private ambulances to transport patients out of area (FOI 224, 2013).
Millions spent on a redundancy programme during a recruitment crisis
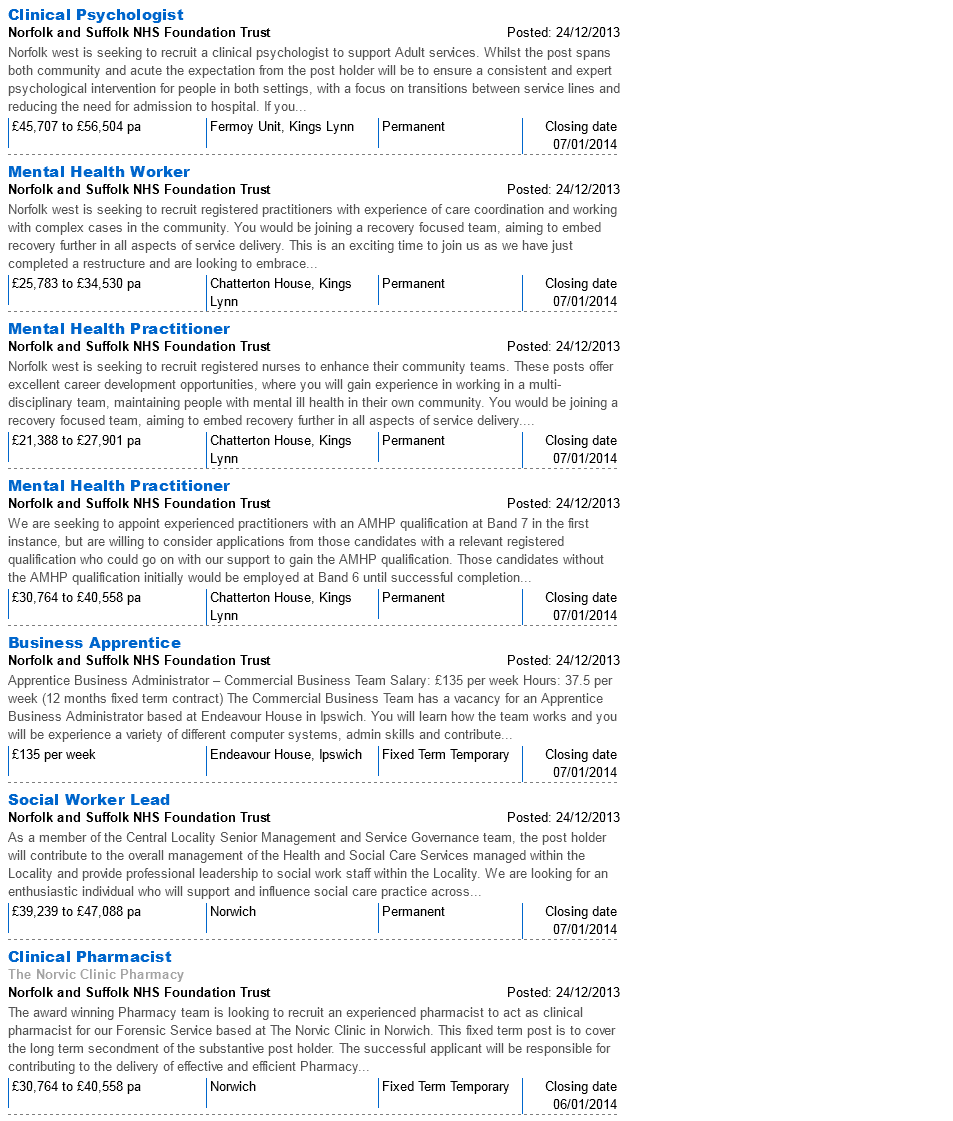
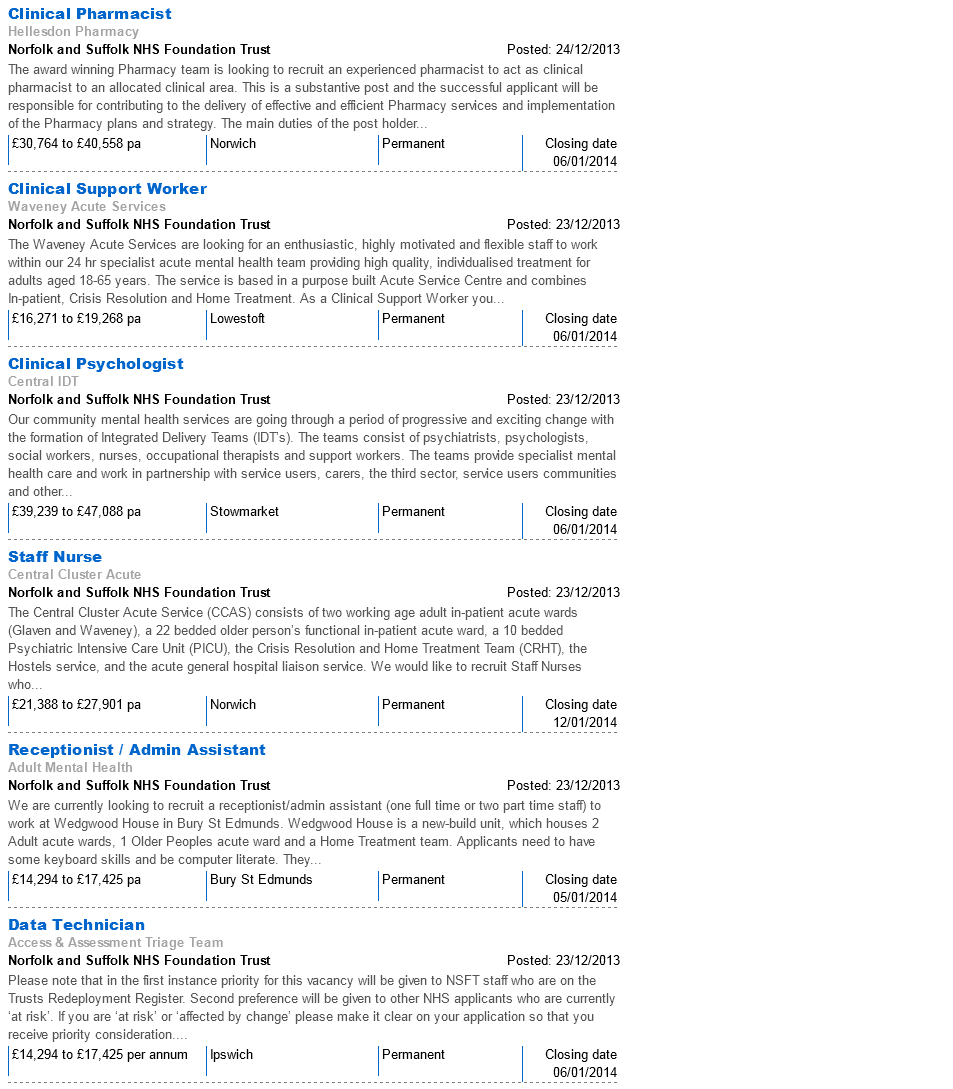
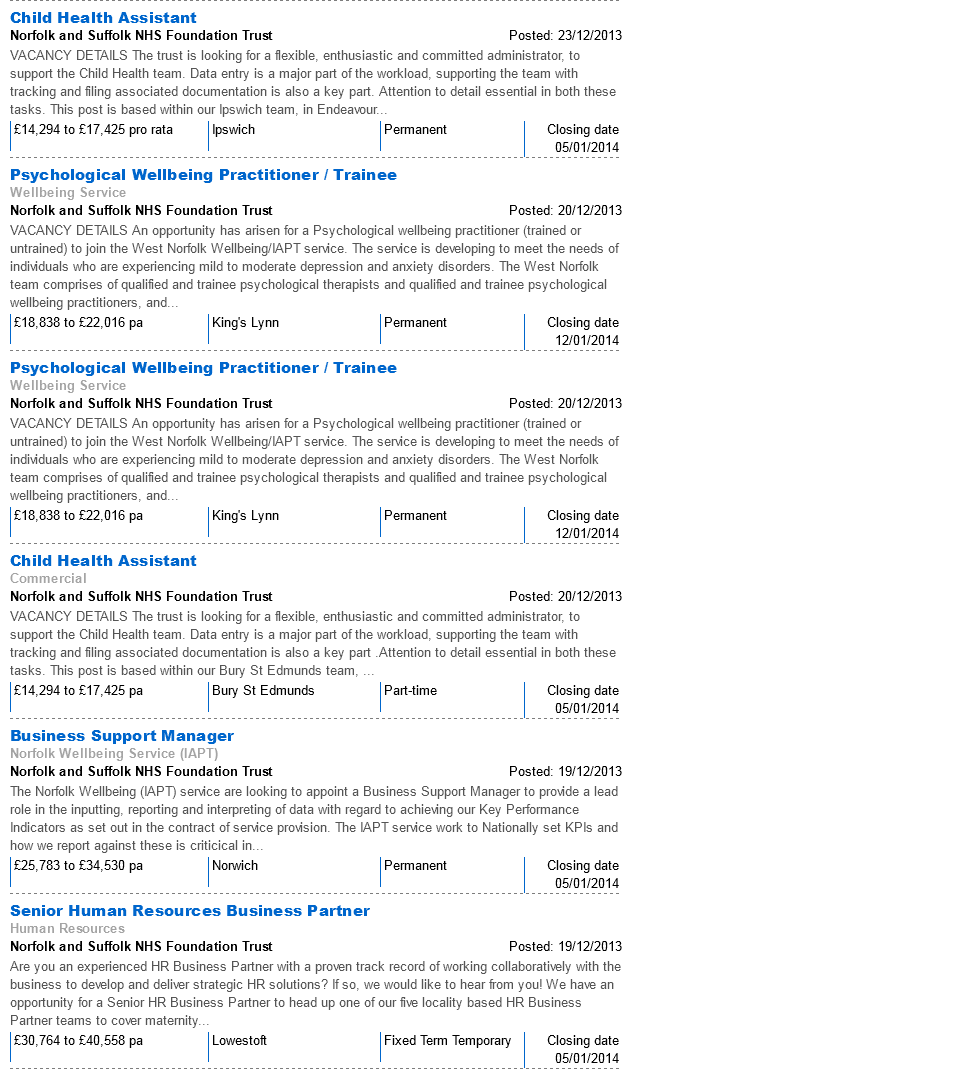
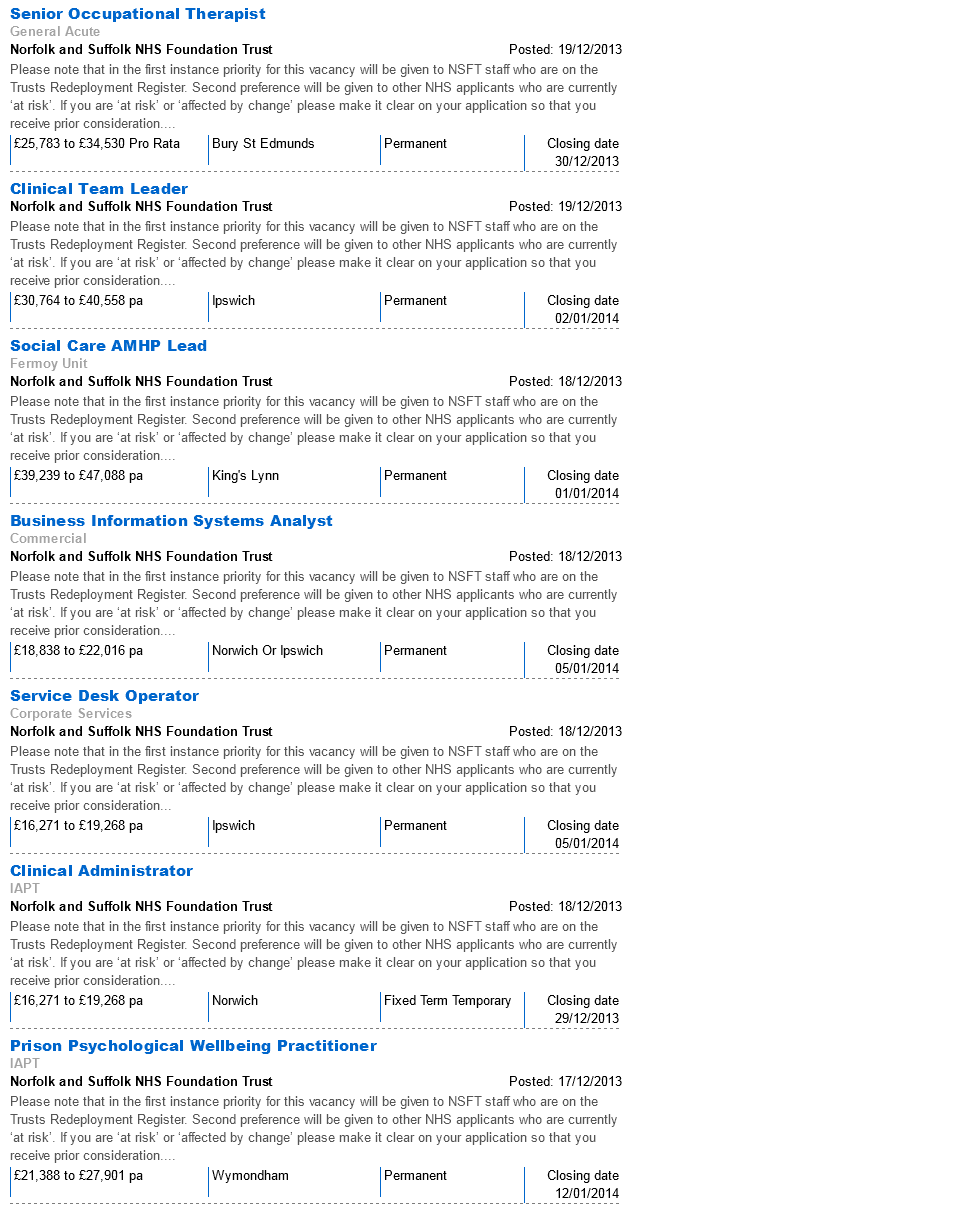
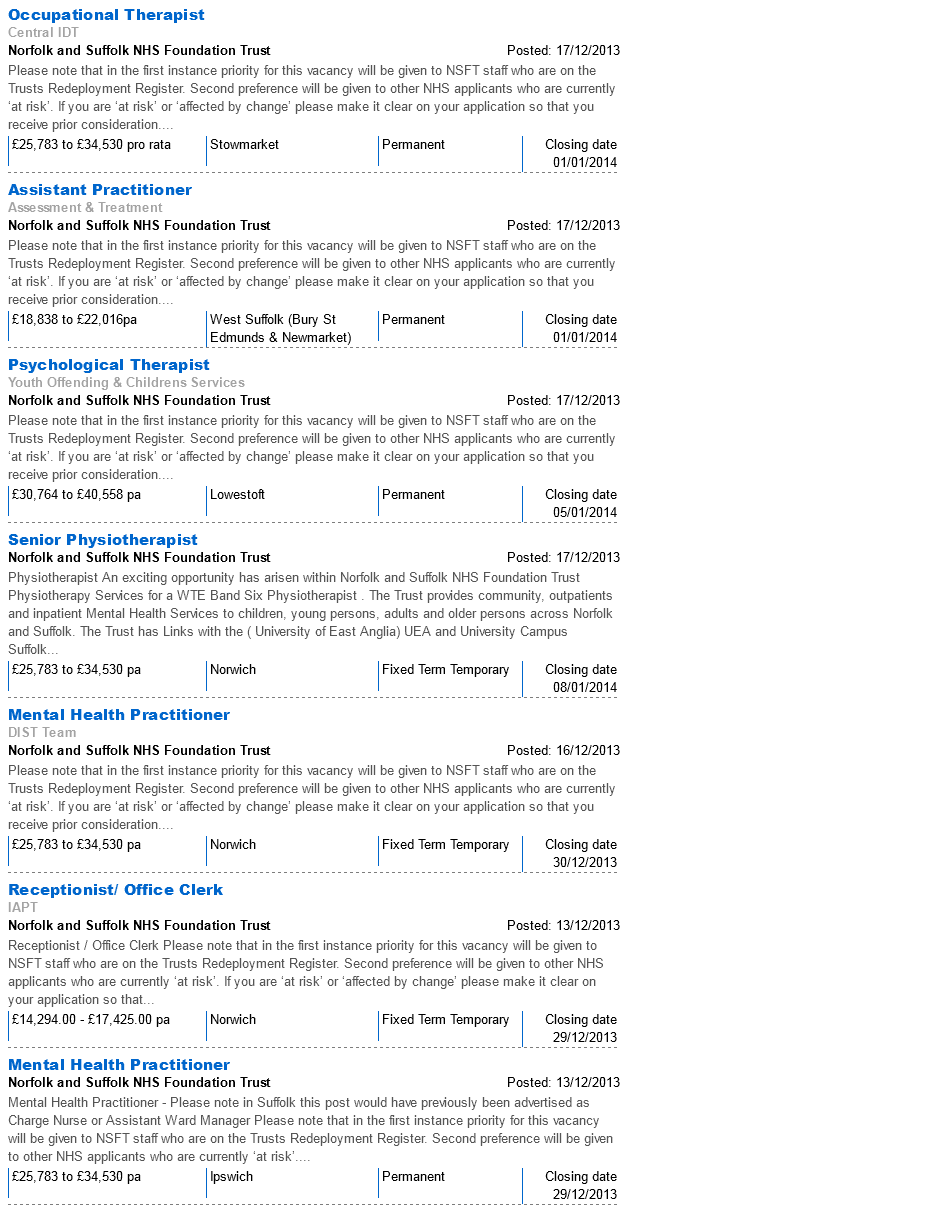
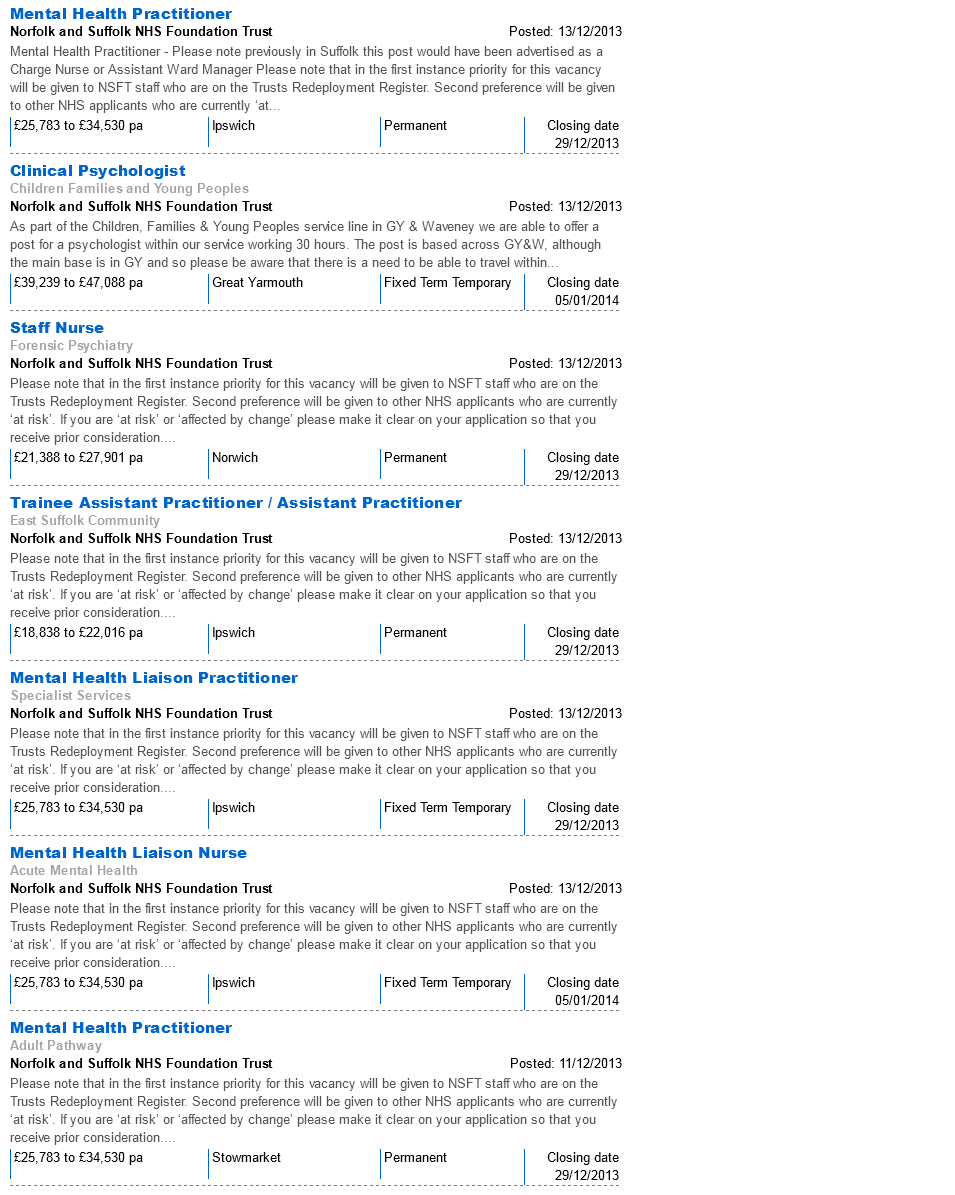
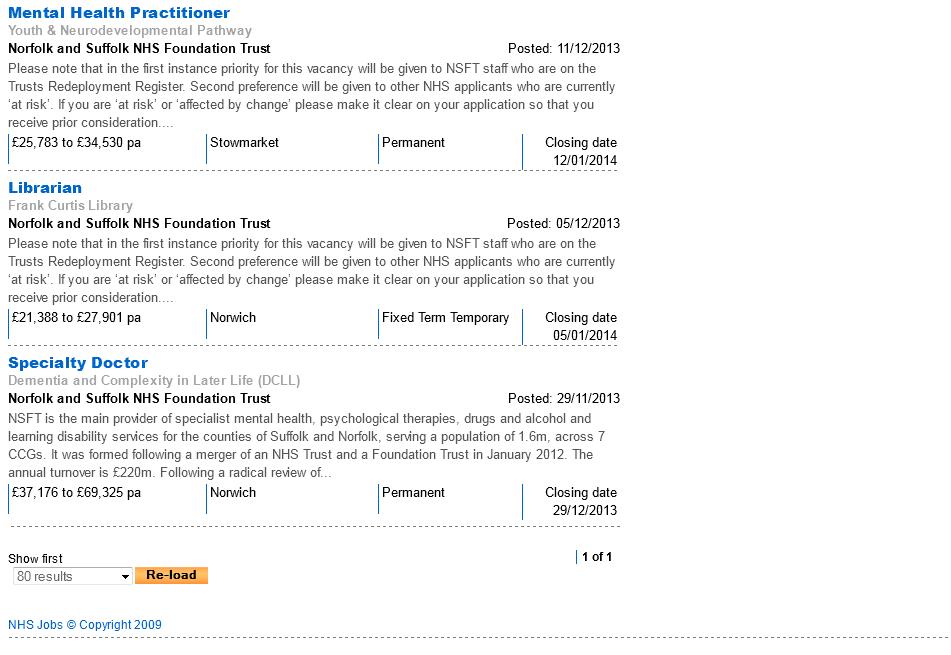
Fifthly, whilst spending all this money on temporary staff and starting a recruitment programme, NSFT has run a poorly implemented and unnecessary voluntary redundancy scheme. Whistleblowers have informed us that the cost of this programme is at least £4 million. It is vital that HOSC discovers the cost of this voluntary redundancy programme and where the money is going to come from. 79 staff were told that they would receive voluntary redundancy and not to apply for their own jobs or equivalent during the ‘radical redesign’ reorganizations. Later, after their own jobs or equivalents were filled by others, NSFT discovered that it needed staff and could not afford the redundancy programme, so it arranged a meeting at which the Acting Chief Executive tried to announce the withdrawal of the voluntary redundancy programme and tried to promote ‘new opportunities.’ The Acting Chief Executive was prevented from giving his presentation for more than an hour, senior managers left the meeting in tears, and staff refused to sign for the new consultation packs and threatened legal action. Shortly afterwards, NSFT changed its position and reinstated the voluntary redundancy programme which the vast majority of the staff involved have taken, leaving between the end of 2013 and April 2014. While NSFT spends millions on voluntary redundancy, as of 28/12/15, NHS Jobs was simultaneously carrying 45 advertisements from NSFT, some for more than one position available (appended to this paper).
FOI Request 01, 2014
Please can you supply for Norfolk Central & West, Norfolk East and Suffolk AATs:
a) Budget and performance against budget (i.e. actual spend) on whatever temporal bases (quarterly, monthly, weekly, etc.) are readily available
b) Performance data against Trust targets/KPIs (including but not limited to ‘scoreboard’ data as leaked to Bob Blizzard and discussed by Kathy Chapman in press) from operational start to as current as possible on whatever temporal bases are readily available – e.g. % seen within target, average waiting time.
c) Reports supplied to CCGs regarding AAT performance
d) Number of queries/complaints received by AAT on whatever temporal basis is readily available and if possible category of complaint/query
e) Internally/externally produced reports into strategy/performance/future of AAT
f) Emails/correspondence from NSFT staff expressing concerns about resourcing/staffing/performance/safety of AAT.
g) Any risk/incident reports registers relating to AAT.
Given that most of this data should be electronically recorded and available and known to AAT and operational management, it should not exceed the 18 hour limit. If you believe this will take more than the 18 hour limit, please let us know asap and we will refine/split. Happy to receive the data in a raw, unrefined format if this makes supply quicker.



It is in reality a great and helpful piece oof info. I’m satisfied tat you simply shared this useful information with
us. Please keep us up to dqte like this. Thank you for sharing.
Feel free to surf to my webpage; GestióN Del Cambio
Excellent post. I am going through some of these issues as well..
Check out my website … vpn special coupon
Appreciation to my father who shared with me on the topic of this weblog,
this website is genuinely amazing.
My web blog: vpn special code
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored material stylish.
nonetheless, you command get bought an nervousness over that you
wish be delivering the following. unwell unquestionably
come further formerly again since exactly the same nearly very often inside case
you shield this increase.
Feel free to visit my homepage vpn special code
This is my first time go to see at here and i am truly pleassant to read all at single
place.
Have a look at my blog post: vpn coupon 2024
My relatives always say that I am killing my time here at web, except
I know I am getting familiarity everyday by reading such fastidious content.
Feel free to visit my page :: vpn special code