It has long been clear that Norfolk & Suffolk NHS Foundation Trust (NSFT) tries to manipulate its inappropriate out of area placement (OAP) bed statistics when the Care Quality Commission (CQC) comes to inspect. As the graph below shows, out of area bed usage was again artificially reduced in the run-up to the latest full CQC inspection during October 2019, only to rise again shortly thereafter, even following NSFT’s blatant attempt to fiddle the most recent figures by excluding £560 per night beds at the remote private hospital on the site of the repeatedly-inadequate Mundesley Hospital which was forced to close by CQC, Southern Hills, on the basis that these placements are not inappropriate since a manager from NSFT visits the site twice per week:
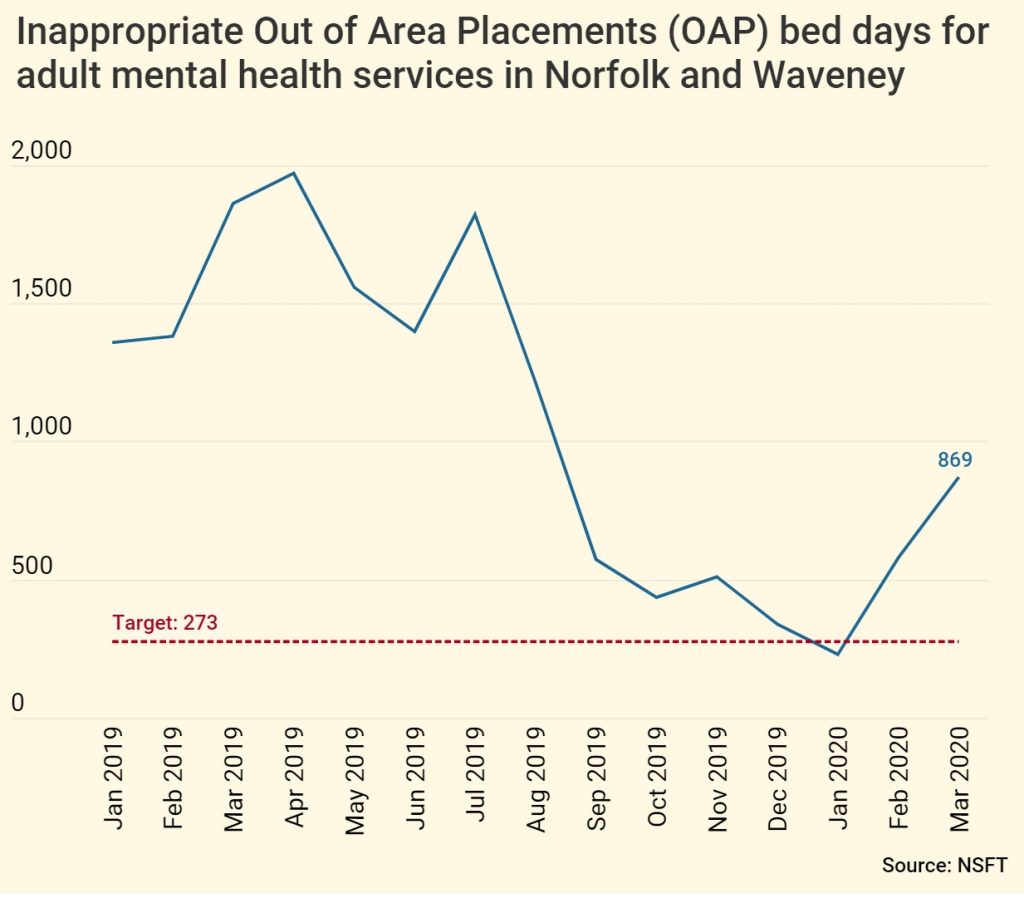
There is a bed crisis because NSFT closed at least 139 of its mental health beds at the same time as its community mental health services were slashed and specialist services were closed. NSFT has recently reopened sixteen beds but these are nowhere near enough to address the beds crisis, particularly when community services remain chronically underfunded. NSFT’s Board and senior management consistently finds the money for new management posts, promotions and pay rises for themselves, relatives and friends but doesn’t seem to care about the quality of mental health services received by the people of Norfolk and Suffolk.
Now, whistle-blowers have provided us with the latest so-called ‘Bed Management Escalation Process’ for central Norfolk, the heart of the beds crisis under the so-called ‘leadership’ of Andy Mack, the brother of the so-called ‘manager’ of repeatedly-inadequate mental health services for Children, Families and Young People (CFYP), Rob Mack. Between them, this particular band of brothers is trousering more than £150,000 per annum from NHS coffers. We and many front line staff have no confidence in either of them. They should be sacked without compensation. You can bet the manager pretending to be Clinical Director, Claire Lussignea, will have been utterly ineffective in representing clinicians and patients in the formulation of this process because ineffective is what she has been ever since she played a central role in the radical redesign disaster.
The ‘Bed Management Escalation Process’ shows how, once mental health professionals have made the clinical decision that a person needs an admission to hospital, trust managers put bureaucratic barriers and delays in the way to stall and prevent admissions; how people are treated differently when no trust bed is available; and how bureaucratic targets override clinical priorities. And this after the delays we know the lack of beds causes to the section assessment process, as Approved Mental Health Professionals (AMHPs) are understandably loathe to arrange Mental Health Act assessments in the absence of available beds: section papers cannot be legally completed without the destination hospital being named and AMHPs are supposed to stay with patients and families until a bed is found, which can take days. CTO recalls often take days and have sometimes taken many weeks.
Here is what is supposed to happen in the fortunate event that there is a bed available at NSFT:
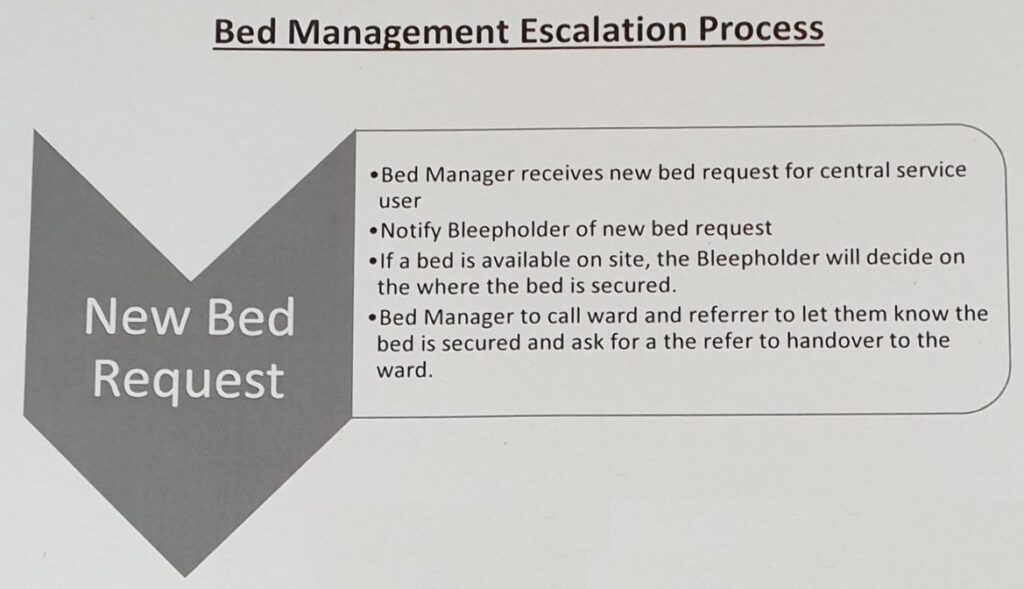
This is pretty much what would be expected. We’re reasonably happy with this: it is what should happen every time because NSFT should have enough beds of its own. So far, two managers are involved who haven’t met the patient (Bed Manager and Bleepholder).
But what happens if there isn’t a bed at central services, i.e. Hellesdon Hospital?
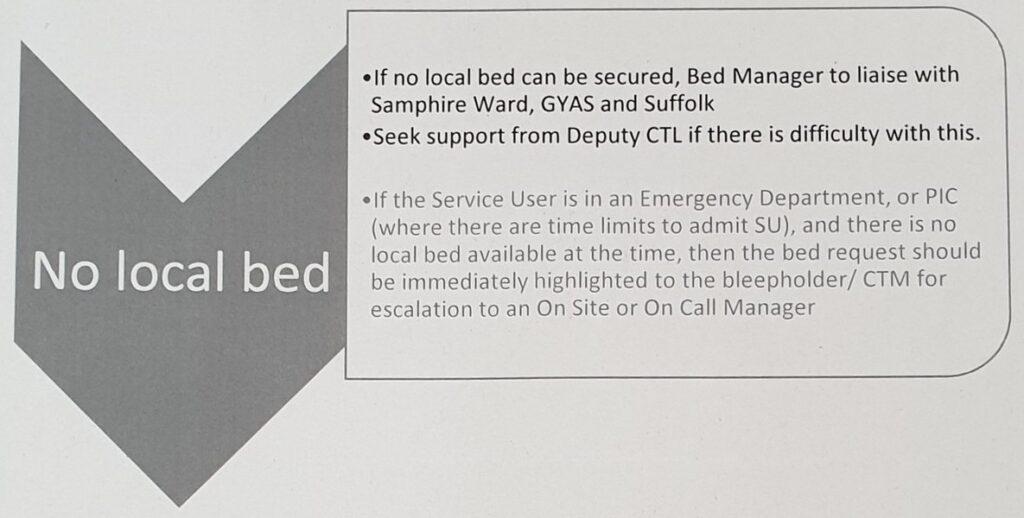
If there is no local bed, NSFT managers will try to find a bed in King’s Lynn, Great Yarmouth or Suffolk. We know that many people in Suffolk and North East Essex believe that their beds should not be used to hide the lack of beds commissioned by Norfolk & Waveney – in fact, Suffolk would replace NSFT as its provider if it could.
None of these distant solutions are acceptable to us, as the beds are not local and should not be routinely used, but they are. Yet another manager will be involved if there are problems. There are now at least three managers who haven’t met the patient involved (Bed Manager, Deputy CTL and Bleepholder/CTM) but not enough beds.
But, if the person in need of admission is in an environment which has a target attached to it, such as Accident & Emergency or in a police cell (PIC), they receive preferential treatment not because of clinical need but to fiddle the figures as the bed request is escalated to yet another manager. There are now at least four managers who haven’t met the patient involved (Bed Manager, Deputy CTL, Bleepholder/CTM and On site/call Manager) but still no bed.
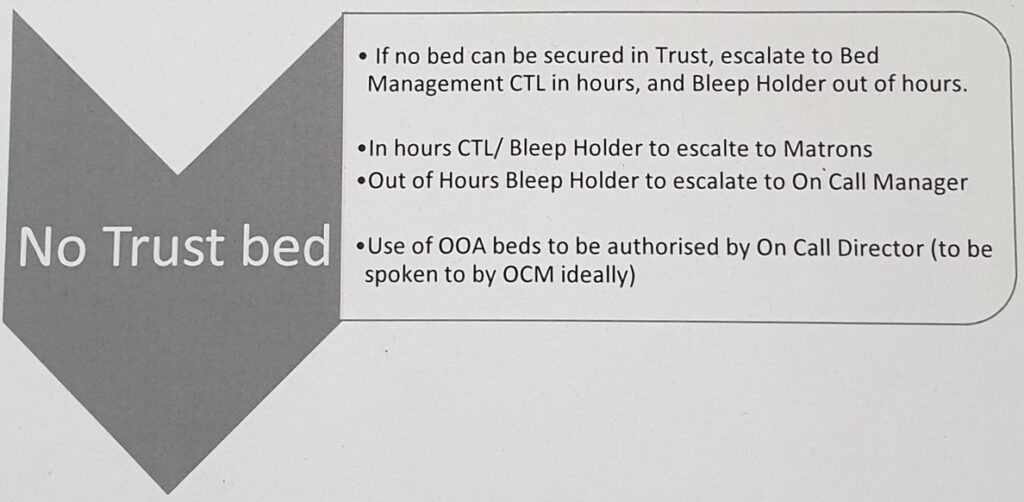
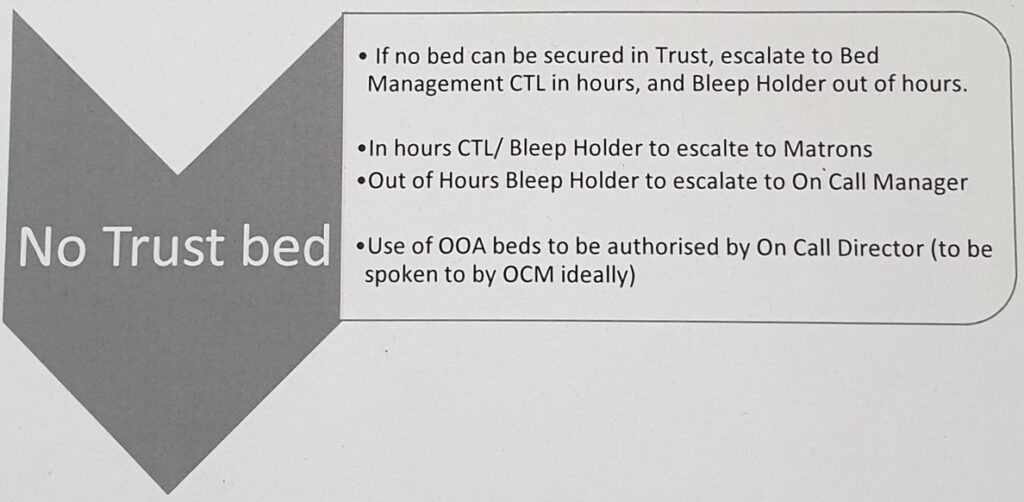
After hours of delay and confirmation that there is no bed available, the issue will be escalated to the CTL/Bleepholder, Matrons/on Call Managers.
If they can’t pressure clinicians to discharge somebody else who wasn’t going to be discharged, sometimes homeless or to some random Bed & Breakfast miles away from their home and community mental health team, frequently very ill and with little to no discharge planning, to empty a bed for the new admission, they will eventually call an On Call Director to authorise the use of an Out of Area bed.
There are now at least five managers who haven’t met the patient involved (Bed Manager, Deputy CTL, Bleepholder/CTM, On site/call Manager and On Call Director) but still no bed. What do any of these managers add to the process, other than delays and costs, given that a clinical decision to admit has already been taken?
The On Call Director could be the £120k+ p.a. Finance Director, Daryll Chapman, a public sector accountant with no professional mental health qualifications.
Alternatively, it could be the new £120k+ Deputy Chief Executive of NSFT who doesn’t work for NSFT and whose LinkenIn says he lives in Kent, Mason Fitzgerald, who spent a staggering seven years accumulating two bachelors degrees in commerce and law and a masters degree in international business from not exactly top-rated academic institutions. Fitzgerald has subsequently added a risk management diploma, a Foundation Certificate in HR and a qualification for company secretaries. Mason Fitzgerald doesn’t work in commerce, the law, international business, HR, risk management or as a company secretary at NSFT. The only qualification Mason Fitzgerald seems to lack is in the area that would be most useful to him when making decisions about out of area beds: professional mental health. At least his massive ELFT salary will help him pay off his eternal student debts.
While whether ‘there are time limits to admit a SU’ influences the process, the physical and mental health needs of the patient do not. Patients are transported across the country by NSFT like low-value parcels or sometimes like wild animals in cages in vans without windows. There is no mention of medical examinations, risk assessments or support networks in this process. More care is taken by suppliers shipping seafood from Billingsgate or flowers from Holland. SU might as well stand for Shipping Unit as Service User. All we need to do is remember how Peggy Copeman or Neil Jewell died.
NSFT needs more front line staff, more local NHS beds and far fewer bureaucrats.
A clinically-led trust with decent values would not look like this.
Good post and straight to the point. I am not sure if this is truly the best place to ask but do you people have any thoughts on where to employ some professional writers? Thanks in advance 🙂
I am really impressed together with your writing skills and
also with the structure for your blog. Is this a paid
topic or did you modify it yourself? Anyway keep up the excellent quality writing, it is rare to look a great weblog like this one today..
Also visit my webpage … vpn special coupon code 2024
Excellent article. Keep posting such kind of info on your site.
Im really impressed by it.
Hey there, You have performed a fantastic job. I’ll certainly digg it
and individually suggest to my friends. I’m sure they’ll be benefited from this site.
my website :: vpn special code
I was wondering if you ever considered changing the structure of your website?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one or two pictures.
Maybe you could space it out better?
My site: vpn special coupon code 2024
Excellent items from you, man. I have remember your
stuff prior to and you are just too excellent.
I really like what you’ve obtained here, certainly like what you
are saying and the way in which by which you assert it.
You’re making it entertaining and you still take care of to keep it
wise. I can’t wait to read far more from you. This is really a tremendous web site.
Stop by my web site vpn special
I’m really enjoying the design and layout of your website.
It’s a very easy on the eyes which makes it much more enjoyable for me to
come here and visit more often. Did you hire out a developer to create your theme?
Fantastic work!
Also visit my website vpn code 2024
I have to thank you for the efforts you have put in penning this site.
I’m hoping to check out the same high-grade blog posts by you later on as well.
In truth, your creative writing abilities has motivated me to get my
own blog now 😉
Check out my web-site – vpn special code
It’s a shame you don’t have a donate button! I’d without a doubt donate to this outstanding blog!
I suppose for now i’ll settle for bookmarking and adding your RSS feed
to my Google account. I look forward to brand new updates and will share this website with my Facebook group.
Chat soon!
My web blog vpn code 2024
Actually when someone doesn’t be aware of afterward its up to other
visitors that they will assist, so here it occurs.
My site … vpn special coupon
What Is Sugar Defender? Sugar Defender is a natural blood sugar support formula created by Tom Green. It is based on scientific breakthroughs and clinical studies.
Wow that was strange. I just wrote an very long comment but after I
clicked submit my comment didn’t appear. Grrrr… well
I’m not writing all that over again. Anyways, just wanted to
say superb blog!
Also visit my web site vpn special coupon
I was suggested this web site by my cousin. I’m not sure
whether this post is written by him as nobody else know such
detailed about my trouble. You are incredible! Thanks!
My blog: vpn special code
I’d always want to be update on new content on this site, bookmarked! .
Wow, superb blog structure! How lengthy have you ever been running
a blog for? you make blogging look easy. The overall glance of your web site is
magnificent, let alone the content material! You can see similar here ecommerce
I like what you guys are up too. Such smart work and reporting! Keep up the superb works guys I have incorporated you guys to my blogroll. I think it will improve the value of my web site 🙂
We are a group of volunteers and starting a new scheme in our community. Your web site offered us with valuable info to work on. You have done an impressive job and our entire community will be grateful to you.
Online medicine home delivery https://indiaph24.store/# india pharmacy
top online pharmacy india
mexico drug stores pharmacies: Mexican Pharmacy Online – mexican drugstore online
Super-Duper site! I am loving it!! Will come back again. I am taking your feeds also.
I believe other website proprietors should take this internet site as an model, very clean and superb user genial style and design.
I truly appreciate this post. I have been looking all over for this! Thank goodness I found it on Bing. You have made my day! Thx again
Hey there! I know this is kinda off topic however I’d figured I’d ask. Would you be interested in exchanging links or maybe guest authoring a blog article or vice-versa? My website goes over a lot of the same subjects as yours and I feel we could greatly benefit from each other. If you are interested feel free to shoot me an email. I look forward to hearing from you! Excellent blog by the way!
awesome
buy medicines online in india Generic Medicine India to USA indian pharmacy online
Do you have a spam issue on this blog; I also am a blogger, and I was wanting to know your situation; we have created some nice methods and we are looking to exchange strategies with others, be sure to shoot me an e-mail if interested.
Thank you for another informative blog. The place else may just I am getting that kind of information written in such an ideal manner? I have a project that I am simply now running on, and I have been at the glance out for such information.
http://mexicoph24.life/# medicine in mexico pharmacies
mexican rx online: Online Pharmacies in Mexico – medication from mexico pharmacy
Can I just say what a reduction to seek out somebody who really is aware of what theyre speaking about on the internet. You undoubtedly know easy methods to deliver an issue to light and make it important. More folks must read this and perceive this side of the story. I cant believe youre no more fashionable because you definitely have the gift.
top 10 online pharmacy in india http://indiaph24.store/# mail order pharmacy india
top 10 online pharmacy in india
canadian pharmacy online store northwest pharmacy canada legal to buy prescription drugs from canada
Some really nice and useful info on this internet site, likewise I conceive the pattern has fantastic features.
cytotec pills buy online buy cytotec online fast delivery Abortion pills online
Boostaro is one of the dietary supplements available in the market that caters to men with erectile dysfunction and sexual health issues.
zestoretic generic: generic zestoretic – generic lisinopril
http://finasteride.store/# generic propecia online
buy propecia without prescription generic propecia no prescription buying generic propecia tablets
Emperor’s Vigor Tonic is a clinically researched natural male health formula that contains a proprietary blend of carefully selected ingredients. It contains minerals and essential nutrients that improve blood circulation and enhance overall health. The Emperor’s Vigor Tonic energy booster supports male health by addressing a specific enzyme in your body that can boost blood flow and nitric oxide production.
http://nolvadex.life/# tamoxifen medication
I really like your writing style, excellent information, thanks for posting :D. “In university they don’t tell you that the greater part of the law is learning to tolerate fools.” by Doris Lessing.
I haven¦t checked in here for some time since I thought it was getting boring, but the last several posts are good quality so I guess I will add you back to my daily bloglist. You deserve it my friend 🙂
http://lisinopril.network/# lisinopril 5 mg medicine
where can i buy cipro online: buy cipro – purchase cipro
cytotec buy online usa buy cytotec pills buy cytotec over the counter
lisinopril 20 mg online how much is lisinopril 40 mg lisinopril 25mg tablets
http://lisinopril.network/# lisinopril price without insurance
generic propecia: buying generic propecia for sale – order cheap propecia prices
Thanks for sharing excellent informations. Your site is so cool. I’m impressed by the details that you have on this website. It reveals how nicely you perceive this subject. Bookmarked this website page, will come back for more articles. You, my pal, ROCK! I found simply the information I already searched everywhere and just could not come across. What an ideal website.
I’ve learn some excellent stuff here. Definitely value bookmarking for revisiting. I surprise how a lot effort you set to make this kind of fantastic informative website.
http://lisinopril.network/# lisinopril 40 mg tablet price
CEREBROZEN aims to improve your hearing naturally. By taking drops of CEREBROZEN’s highly concentrated liquid formula daily, you can purportedly support healthy hearing and boost overall ear health.
zestril 20 mg tab lisinopril 80mg tablet buy lisinopril online uk
https://nolvadex.life/# tamoxifen mechanism of action
I’ve been surfing online greater than three hours these days, yet I by no means discovered any attention-grabbing article like yours. It¦s pretty worth sufficient for me. In my opinion, if all web owners and bloggers made just right content as you did, the internet can be a lot more useful than ever before.
ciprofloxacin: ciprofloxacin over the counter – ciprofloxacin order online
I very happy to find this website on bing, just what I was searching for : D also bookmarked.
http://ciprofloxacin.tech/# cipro ciprofloxacin
buy cytotec over the counter: Abortion pills online – buy cytotec
aromatase inhibitor tamoxifen tamoxifen hair loss tamoxifen breast cancer prevention
http://finasteride.store/# cost generic propecia pills
http://cytotec.club/# buy cytotec online fast delivery
get cheap propecia no prescription: cheap propecia pills – get propecia