Norfolk and Suffolk NHS Foundation Trust (NSFT) sent dishonest letters to hundreds of children and young people on waiting lists.
NSFT claims that the dishonest discharge letters were a ‘mistake’ but refused to answer the BBC’s reasonable questions about what happened and what it is doing about put things right. We don’t even know what the ‘mistake’ was. We suspect the ‘mistake’ was getting found out.
What has been going on?
At the end of February 2020, the CQC inspected the Youth Service of mental health services for Children, Families and Young People (CFYP) at NSFT.
It was disastrous. Not just for waiting lists but it is waiting lists on which we will focus below.
CQC found:
We were not assured that processes for managing waiting lists, particularly team-held waiting lists, kept people safe. Where a patients’ risk was discussed in team meetings and there was an identified change to risk, we saw that risk assessments were not always updated. There was no clear process to ensure patients on team-held waiting lists were appropriately monitored and supported. We saw large gaps in records, with one patient not having had direct contact since July 2019. Patient waiting list concerns had been mentioned at the last four inspections and it was disappointing that this had not been fully addressed within this team.
So, CQC had expressed concerns at the last FOUR inspections.
There was no clear process to ensure patients on teamheld waiting lists were appropriately monitored and supported. We saw gaps in records; one patient had not been contacted since July 2019. Another patient had several attendances at the acute hospital emergency department whilst waiting for allocation, the GP had followed up with concerns and in the summer of 2019 the liaison staff at the Accident and Emergency department submitted an incident report due to the lack of availability for support from the youth team. A further patient had been referred to the team in March 2019. The patient was added to the waiting list for a care co-ordinator in July 2019 but only made it to the priority meeting in January 2020. We were not assured that processes for managing waiting lists, particularly team-held waiting lists, kept people safe.
This mismanagement has serious, perhaps fatal, consequences:
We reviewed the early learning report from a recent serious incident. We saw that at the time of the incident, the patient had recently been seen by clinicians. However, in the months prior to this we saw missed opportunities to engage with the patient, cancelled appointments and cancelled group sessions due to staff sickness. We saw evidence of a decline in the patients mental health that was not immediately acted upon. The patient was on the teamheld list and did not have one single clinician overseeing their care. This is currently subject to a full root cause analysis investigation that has not yet been completed.
Front line NSFT staff told CQC that there were not the resources to provide a service to those on waiting lists:
The staff member was concerned that the team was expected to address the waiting list for assessment without the resource in place to then offer support identified in this process.
We believe the despicable and dishonest decision to discharge hundreds of children and young people, rather than provide the resources and competent management to deliver promised care to them, was made by the leadership of the CFYP Care Group and the operational management of NSFT, probably with knowledge and approval of the executive Board. It also appears likely that the local representatives of CQC were aware of what NSFT was doing.
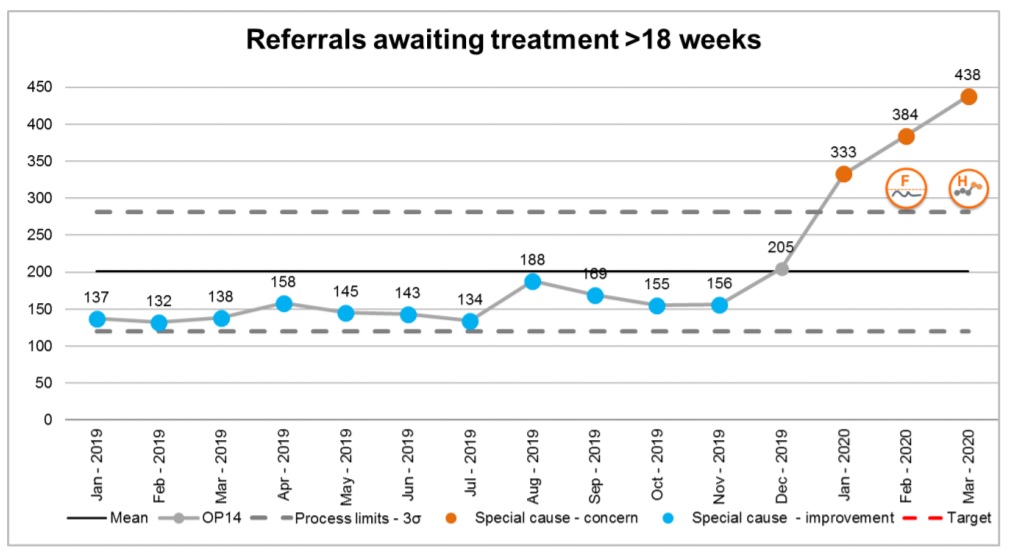
NSFT’s latest Board papers let us see what was happening to waiting lists in CFYP around the time of the CQC inspection in February 2020:
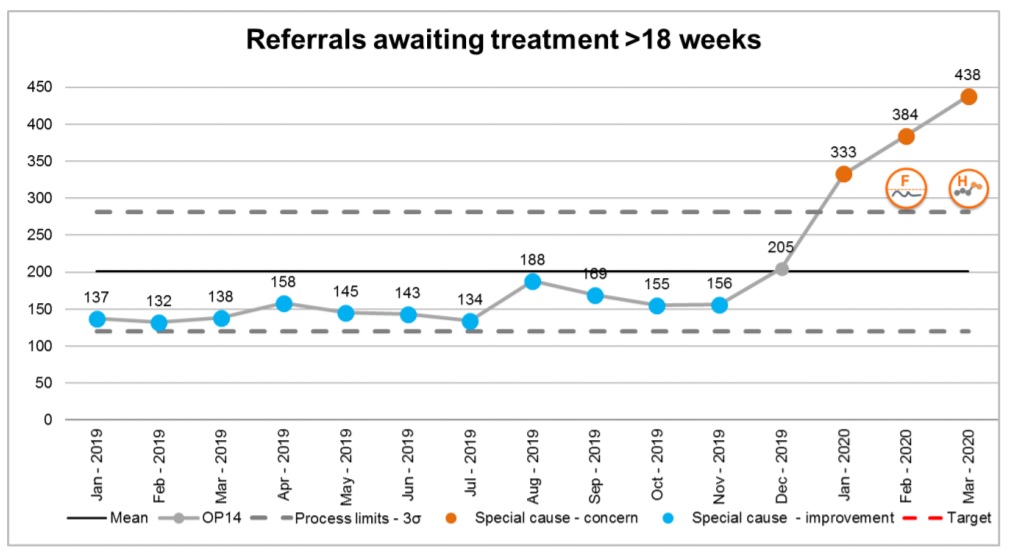
The ‘Integrated Performance Report’ states:
225 (51.4%) relate to CFYP services in Norfolk and Waveney, up 19 from 206 in February 2020… the system will be expected to consistently fail this target and that performance is now reporting as a cause for concern in special cause variation.
So, more than half of all breaches of the 18 weeks waiting time limit were due to CFYP in Norfolk and Waveney. Even before the CQC inspection, NSFT’s Board knew the serious problems were endemic in CFYP.
The February 2020 CQC inspection report tells us:
In response to the concerns raised within this report, the trust leadership team provided assurance of action which had begun just prior to the inspection. For instance, on 13 February 2020, an executive-led rapid improvement board had been established. This aimed to accelerate improvements and have senior leadership oversight.
NSFT’s ‘trust leadership team’ and an ‘executive-led rapid improvement board’ with ‘senior leadership oversight’ must have known of and approved the plan to discharge hundreds of children and young people from waiting lists.
The CQC inspection report also tells us that:
The care group leadership team were spending 4 to 5 days per week at St Stephens Road. We were told of plans to undertake a large-scale clinical review of the waiting list early in March 2020.
It seems impossible that the care group leadership team could have been unaware of the decision to abuse the Covid-19 epidemic to dishonestly discharge hundreds of children and young people from waiting lists for treatment, given they were spending four to five days per week at 80 St Stephen’s and told the CQC of their plans ‘to undertake a large-scale clinical review of the waiting list’. Indeed, the ‘Advice and Signposting Team’ which was supposed to help discharge the children and young people without promised treatment is widely acknowledged to be the ‘baby’ of the CFYP Service Director, Rob Mack. We’ve already said that Rob Mack should be sacked.
The care group leadership reported to Amy Eagle, the disgraceful appointment as £90k+ Deputy Chief Operating Officer of NSFT, who has an appalling track record of closing and cutting services at 80 St Stephen’s. Eagle reports to Stuart Richardson, the £120k+ Chief Operating Officer of NSFT, who has created chaos in his nearly two years at NSFT. It seems inconceivable that Eagle and Richardson did not know what was going on at 80 St Stephen’s. If they knew, they were complicit; if they didn’t know they were incompetent. Both have outstayed their welcome at NSFT. In fact, neither should have been employed in the first place.
It appears that even NHS Improvement has lost patience with Eagle, Richardson and the NSFT Board. We were told that there would no longer be an Improvement Director when Marie Gabriel and former Professor Warren were installed as Chair and Chief Executive as NSFT ‘no longer needed one’. However, the May 2020 Board papers tell us:
An Improvement Director has been appointed with NHSI to support the trust and will focus initially on CFYP.
The new ‘Director of Improvement’, James Innes, a pharmacist, has just completed a health leadership masters and looks far below the calibre of previous Improvement Director, Alan Yates. But he wouldn’t have to do much to be an improvement on Yates’ successor as Improvement Director, Philippa Slinger. But will he have the skills, experience and authority to challenge the appalling and inept but devious and self-serving management clique at NSFT?
What did the rest of the NSFT Board know?
What were the Chief Nurse, Diane Hull, and Chief Medical Officer, Dan Dalton, doing while all this was going on?
What did CQC know?
Is this what ‘improvement’ looks like?
How much longer can children and young people be made to pay the price of the NSFT Board’s incompetence?
There is more to tell and many more questions for NSFT to answer.
Stay tuned.
The point of view of your article has taught me a lot, and I already know how to improve the paper on gate.oi, thank you. https://www.gate.io/fr/signup/XwNAU
thank you very much
_________________
???????? ????
«????? ?????»: ??? ???????? ??????? ? ????????????? ? ???????
??????????????? ? ???? ??
?????? ????????
«????? ?????» ??????????????? ???? ??? ??????? ????????? ? ??????? ????????????? ? ??????? ? ??????.
?? ?????????? ????? 6 ??? ?? ??????? ????????? ??????? ????????? ?????????,
???????? ?? ??????????????? ????? ??????? ?? ????? ???
50 ??????????????????????? ????????????.
???? ???????? ????????????? ?????? ?????? ???????????? ?????, ??????? ?? ????????? ????? ? ?????????? ????????
??????????? ????????.
??????? ????????: ???????? ???????? ????????
???? ???????????? – ??? ?????? ????????,
?? ???????????????? ?????? ? ????????????? ?????? ? ?????? ????????? ??? ????????????? ?????????? ???????? ?????????? ?????.
?? ?????? ??????? ?????? ? ???????????? ???????????? ??
?????? ???????.
??????? ?????? ?????: ?? ?
?? ?
?? ?????????? ????????????? ??????,
???????:
????????? ??????: ???????????
??????????? ????? ?? ?????????????;
??????????-???????????? ??????:
??????? ? ?????????? ???????????
??????????;
???????? ? ?????????? ???????: ??????? ? ??????? ????? ?????????? ?????;
??????????? ?????? ? ??????????: ???????????? ?????????? ?????? ???????;
????????? ? ??????????????? ??????: ???????? ?????? ??? ?????? ???????;
?????? ? ???????? ????????????:
???????????????? ?????? ? ??????????? ????????.
?????????????? ?????? ? ??????? ???????
?? ???????? ? ?????????? ??????????? ??????????, ??
??????? ??? ?? ??????? ???????????? ???????????.
??? ?????? – ??? ?????????? ??????????? ????? ????? ??? ??????? ???????, ????????
??? ?????????? ? ?????.
???????? ??????? ??????????????
?????????? ???????? ???? ? ?????? ???????
??????. ???? ??????? ????? ??????????????? ?????????? ??????????,
??????? ?? 43% ?? ?????? ???????.
???????? ???????? ? ????????????
???? ??????????? ?????? ????????? ?????
???????????? ? ?????? ?????.
?? ??????????? ???????????? ?????????? ?????, ? ?????? ???? ?????????? ? ????????????.
«????? ?????»: ??? ????? ? ??????
???? ?? ????? ???????? ? ??????? ???????????? ? ??????, ??????????? ? «????? ?????».
?? ?????? ??????? ?? ??? ??????
? ??????????? ??? ?????? ?? ?????? ????????????? ?????? ??????.
???????? ?????? ?? ????? ?????, ? ?? ?????????? ???????? ? ????.
??????????????? ? ?????? ????????? ???????? «????? ?????»
??????? ???, ?? ????????? ??????????, ??????????????? ?
????????. ???? ??????? ?????? ????????? ? ????? ??? ??????, ????????? ??? ????????.
Hello, adventurers! Join our Telegram channel for exclusive, uncensored combat footage. Prepare to have your perceptions shattered!
This is unique content that won’t be shown on TV.
Link to Channel: HOT INSIDE UNCENSORED
https://t.me/+PhiArK2oSvU4N2Iy
?? ??????? ??????? ? ????? ????? ?? ???? ????, ???? ???? ? ??? ????????? ?? ????????.
??????? ????? ??????? ? ????????
I want to show you one exclusive program called (BTC PROFIT SEARCH AND MINING PHRASES), which can make you a rich man!
This program searches for Bitcoin wallets with a balance, and tries to find a secret phrase for them to get full access to the lost wallet!
Run the program and wait, and in order to increase your chances, install the program on all computers available to you, at work, with your friends, with your relatives, you can also ask your classmates to use the program, so your chances will increase tenfold!
Remember the more computers you use, the higher your chances of getting the treasure!
DOWNLOAD FOR FREE
Telegram:
https://t.me/btc_profit_search
I want to show you one exclusive software called (BTC PROFIT SEARCH AND MINING PHRASES), which can make you a rich man, and maybe even a billionaire!
This program searches for Bitcoin wallets with a balance, and tries to find a secret phrase for them to get full access to the lost wallet!
Run the program and wait, and in order to increase your chances, install the program on all computers available to you, at work, with your friends, with your relatives, you can also ask your classmates to use the program, so your chances will increase tenfold!
Remember the more computers you use, the higher your chances of getting the treasure!
Thank me by donating if you have the opportunity.
Free Download:
https://t.me/btc_profit_search
???????? ???? ?????/ ?? ??????? ????? ?? ?????? ??????????! ?????????? ???? ????????, ???? ? ?????? ????????.
????? ??????? ? ??????
????? ???????. ? ?????-??????????? ?????? ????????????? ? ???????????. ???????? ?????? — ?? 97% ?? ???????? ?????????. ????? 1 000 000 ??? ? ???? ?????????. ????? ?? ?????? ?? ????????? ????!
???? ????? ?????????? ?? ??????? ????? ??????? ? ????????, ???????? ???????? ?? ????
I’m really enjoying the design and layout of your
website. It’s a very easy on the eyes which makes it much more pleasant for me to come here
and visit more often. Did you hire out a designer to create your theme?
Fantastic work!
Here is my homepage: ???????????? ?????? ??????
???????????? ???????????
???????? ???????? ?????????? ????????????? ?? ?????? ??????????? ? ???????? ???? ?????
??????? ????? ??????? ? ??? ? ??
?????? ?? ????????? ?? 95% ????????? ????????. ????? ??????? ?? ????????? ????. ??? ??????? ?? ?????? ????? ?? ????.
????? ???????????? ? ??????? ???
?????? ?? ????????? ?? 95% ????????? ????????. ????? ??????? ?? ????????? ????. ??? ??????? ?? ?????? ????? ?? ????.
?????? ??????? ???
???????? ???? ?????/ ?? ??????? ????? ?? ?????? ??????????! ?????????? ???? ????????, ???? ? ?????? ????????.
??????? ????? ????????? ??????? ? ???
Hello from Happykiddi.
???????????? ???????????
???????? ???????? ?????????? ????????????? ?? ?????? ??????????? ? ???????? ???? ?????
?????? ??????? ? ???
Service for fast indexing of links in Google.
First result in 48 hours. 200 links for FREE.
https://clck.ru/37HzsY
thanks, interesting read
very good
C????? ??? ??????? ?????????? ?????? ? Google.
?????? ????????? ?? 48 ?????.
?? ???? ?????? ?? ????????
200 ?????? ?????????.
????????????? ??????
SpeedyIndex – service for fastened indexing of links in Google.
Before result in 48 hours. 200 links for FREE.
SpeedyIndex
Hey very cool blog!! Man .. Beautiful .. Amazing .. I’ll bookmark your site and take the feeds also…I’m happy to find so many useful info here in the post, we need work out more strategies in this regard, thanks for sharing. . . . . .
I think this is among the most significant information for
me. And i’m glad reading your article. But wanna remark on few general things, The web site
style is great, the articles is really nice : D. Good job, cheers
I will right away snatch your rss as I can not to
find your e-mail subscription link or e-newsletter service.
Do you’ve any? Kindly allow me know so that I may just subscribe.
Thanks.
This blog was… how do you say it? Relevant!! Finally I have
found something which helped me. Thanks a lot!
Also visit my blog – vpn special code
Thankfulness to my father who informed me about this website, this weblog is
actually remarkable.
Here is my blog vpn special coupon code 2024
With havin so much content do you ever run into any issues of plagorism or copyright violation? My website has a lot of exclusive content I’ve either written myself or outsourced but
it looks like a lot of it is popping it up all over
the web without my permission. Do you know any techniques to help prevent content from being ripped off?
I’d genuinely appreciate it.
Feel free to visit my site … vpn special code
You really make it seem so easy with your presentation but I find this topic to be actually something
which I think I would never understand. It seems too complicated and very
broad for me. I am looking forward for your next post, I will try
to get the hang of it!
Here is my webpage – vpn special coupon
Hi there, all is going perfectly here and ofcourse every one is
sharing information, that’s really fine, keep up writing.
Here is my webpage – vpn special
Have you ever thought about publishing an ebook or guest authoring on other
blogs? I have a blog centered on the same topics you discuss and would really like to have you share some stories/information. I know my subscribers would value
your work. If you are even remotely interested, feel free
to shoot me an e-mail.
Check out my website: vpn special code
Greate article. Keep posting such kind of info on your blog.
Im really impressed by your site.
Hey there, You’ve done a fantastic job. I’ll certainly digg
it and personally suggest to my friends. I am sure they’ll be benefited from this web site.
Feel free to visit my site :: vpn special code
??????? ???? ????????? ??????? ???????????? ? ???????????? ???????? ????????.
???????????? ? ??? ????– ?????? ????, ?? ??????? ?? ??????? ??? ???????????!
Only wanna input on few general things, The website layout is perfect, the written content is really wonderful. “To establish oneself in the world, one has to do all one can to appear established.” by Francois de La Rochefoucauld.
I every time used to study paragraph in news papers but now as I am
a user of internet therefore from now I am using net
for content, thanks to web.
My blog; vpn coupon code 2024
Hi there, You have performed a fantastic job. I’ll certainly digg it and in my view recommend to my friends. I’m sure they’ll be benefited from this website.
I saw a lot of website but I conceive this one holds something special in it in it
????? ??? ????????????????????????????????
Wow, amazing weblog format! How long have you ever been blogging for?
you make blogging look easy. The total look of your site
is excellent, as well as the content material! You
can see similar here e-commerce
Wonderful beat ! I would like to apprentice while you amend your web site, how can i subscribe for a blog site? The account aided me a acceptable deal. I had been a little bit acquainted of this your broadcast provided bright clear idea
Hi there very nice website!! Man .. Beautiful .. Wonderful .. I will bookmark your website and take the feeds additionally…I am glad to search out so many useful info here in the post, we need develop extra techniques on this regard, thank you for sharing. . . . . .
Hi there, I found your website via Google while searching for a similar topic, your website came up, it seems good. I have bookmarked it in my google bookmarks.
Online medicine home delivery http://indiaph24.store/# buy medicines online in india
top 10 pharmacies in india
mexican pharmacy: mexican pharmacy – best online pharmacies in mexico
india pharmacy http://indiaph24.store/# india online pharmacy
pharmacy website india
Wow! This can be one particular of the most beneficial blogs We’ve ever arrive across on this subject. Basically Great. I am also a specialist in this topic so I can understand your hard work.
Good write-up, I am normal visitor of one¦s site, maintain up the excellent operate, and It is going to be a regular visitor for a lengthy time.
This is the right blog for anyone who wants to find out about this topic. You realize so much its almost hard to argue with you (not that I actually would want…HaHa). You definitely put a new spin on a topic thats been written about for years. Great stuff, just great!
You have brought up a very good details, thankyou for the post.
I believe you have observed some very interesting points, regards for the post.
???????????? ?????? ????????? ?????? ???????? ?????? ? ??????. ????? ??? ?????????, ??? ??????????????? ???????????!
???????????? ?????? ????????? ?????? ??????? ? ??????. ????? ??? ?????????, ??? ??????????????? ???????????!
???????????? ?????? ????????? ?????? ??????????? ??????? ?????? ? ??????. ????? ??? ?????????, ??? ??????????????? ???????????!
????? ?????? ?? ???????. ????????? ?????? ??? ?????????? ???????? ???? ????? ????????? ??????? ?? ??????????. ??????????? ? ??? ?????????? ?? ?????????? ? ????????? ???? ????????? ?????. ???????? ?? ??????? https://anglijskij-po-filmam.pp.ua/ ? ????????? ????? ?????? ?????? ? ??? ???????????????!
?????????? ???????? ???? ???????? ??????? ??????????? ? ????????????? ??? ??????????? ????? ? ??????? ????? ??????? ? ???????? ?? ?????????? ? ?????????? ??????. ??????????? ????????? ????????, ?????????? ? ????????????? ?????? ? ??????? ?? ????? ?????????. ???? ?????? ? ??????? ?? ?????? ??????? ??? ????????? ????????? ?????, ?? ? ??????? ????????? ?????????? ???? ? ????????. ??????????? ????????? ? ???????? ?????????????? ?????? ????????. ????????? ??? [url=]https://filmy-na-anglijskom-yazyke.pp.ua/[/url]
What’s Going down i am new to this, I stumbled upon this I have discovered It positively useful and it has aided me out loads. I’m hoping to contribute & aid other customers like its aided me. Good job.
india pharmacy mail order indianpharmacy com online pharmacy india
buying prescription drugs in mexico online: cheapest mexico drugs – mexico pharmacies prescription drugs
Keep up the excellent work, I read few posts on this internet site and I believe that your blog is rattling interesting and contains sets of great info .
I like the valuable information you provide in your articles. I’ll bookmark your weblog and check again here regularly. I’m quite sure I will learn a lot of new stuff right here! Good luck for the next!
http://indiaph24.store/# top online pharmacy india
Online medicine home delivery https://indiaph24.store/# top 10 online pharmacy in india
world pharmacy india
I haven’t checked in here for a while as I thought it was getting boring, but the last few posts are good quality so I guess I will add you back to my everyday bloglist. You deserve it my friend 🙂
What’s Happening i’m new to this, I stumbled upon this I have found It positively helpful and it has aided me out loads. I hope to contribute & help other users like its aided me. Great job.
canadian drug pharmacy canadianpharmacy com canadian pharmacy king reviews
What i don’t realize is if truth be told how you are not really much more well-favored than you may be right now. You’re so intelligent. You recognize thus considerably with regards to this subject, produced me for my part believe it from numerous numerous angles. Its like women and men are not involved unless it’s one thing to accomplish with Woman gaga! Your personal stuffs great. Always care for it up!
FitSpresso stands out as a leading weight loss product currently dominating the market. This potent supplement asserts its ability to facilitate healthy weight loss naturally, free from any adverse side effects. Its formulation incorporates clinically studied ingredients that synergistically contribute to promoting natural fat burning, elevating metabolism, and sustaining enduring weight loss.
Prostadine is a 100 natural supplement that helps in ensuring that your prostate remains healthy and functions optimally even as you age. It also helps in reducing symptoms like frequent urination, weak urine stream and urine leakage. With its easy-to-use dropper, you can maintain proper prostate health without any hassle and ensure that you enjoy a healthy life even as you grow older.
http://cytotec.club/# order cytotec online
Nice post. I was checking continuously this blog and I am impressed! Extremely useful info specially the last part 🙂 I care for such information much. I was looking for this certain information for a long time. Thank you and best of luck.
generic propecia price order cheap propecia prices cost of cheap propecia without a prescription
Boostaro is one of the dietary supplements available in the market that caters to men with erectile dysfunction and sexual health issues.
buy propecia no prescription: buy generic propecia no prescription – cheap propecia pill
Sight Care is a 100 natural and safe supplement that was developed after many years of studies by the best scientists, made to solve the nutritional deficiencies of our eyes, rejuvenating and restoring our perfect vision.
cost of brand name lisinopril lisinopril 20 mg price in india lisinopril 50 mg price
Emperor’s Vigor Tonic is a clinically researched natural male health formula that contains a proprietary blend of carefully selected ingredients. It contains minerals and essential nutrients that improve blood circulation and enhance overall health. The Emperor’s Vigor Tonic energy booster supports male health by addressing a specific enzyme in your body that can boost blood flow and nitric oxide production.
http://lisinopril.network/# lisinopril generic over the counter
https://finasteride.store/# get generic propecia pills
Would you be occupied with exchanging links?
buying propecia: order propecia for sale – cheap propecia without prescription
cipro online no prescription in the usa cipro pharmacy cipro
https://lisinopril.network/# lisinopril 10 best price
arimidex vs tamoxifen bodybuilding tamoxifen tamoxifen endometrium
?????, ??? ????? ???????? ???????? ???????? ??????? ?????? ?? ???????? ?????.
Your house is valueble for me. Thanks!…
buy cytotec pills: cytotec pills online – buy cytotec
FlowForce Max stands as a natural dietary formula, crafted through recent technological discoveries to specifically address prostate and urinary concerns in men across various age groups. The male supplement features a formulation derived from natural ingredients sourced from local growers.
https://cytotec.club/# cytotec abortion pill
you have a great blog here! would you like to make some invite posts on my blog?
http://lisinopril.network/# lisinopril 40 mg for sale
tamoxifen and uterine thickening should i take tamoxifen ?»?dcis tamoxifen
The DentiCore supplement is designed to promote healthy gums and teeth through an advanced technique and herbal ingredients. With no negative side effects, it contains only natural components. Its formulation focuses on integrating multiple essential elements crucial for maintaining dental health, ensuring pharmaceutical quality. Produced in a GMP-certified US facility registered with the FDA, DentiCore’s formula is safe for your body, containing only ingredients beneficial to your oral system.
ciprofloxacin 500 mg tablet price: cipro ciprofloxacin – ciprofloxacin generic
Wonderful blog! I found it while browsing on Yahoo News. Do you have any suggestions on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Appreciate it
?????, ??? ????? ?????? ???????? ???????? ??? ?????? ?? ???????? ?????.
https://lisinopril.network/# lisinopril 419
tamoxifen depression how to get nolvadex tamoxifen vs clomid
order cheap propecia: cost cheap propecia no prescription – buying propecia without rx
????????-??????, ??? ????? ?????? ?????????? ???????? ??????????????? ?? ??????? ??????????????.
buy misoprostol over the counter cytotec buy online usa buy cytotec
http://ciprofloxacin.tech/# buy cipro online canada
https://lisinopril.network/# lisinopril 20mg 25mg
????, ??? ??????????? ???????????? ???????? ?????? ??? ????? ?????? ???????, ? ????????? ?? ???? ??????.
cost of tamoxifen: nolvadex steroids – tamoxifen rash
https://lisinopril.network/# where to buy lisinopril online
cytotec online buy cytotec cytotec buy online usa
Some really fantastic information, Glad I discovered this. “Things we not hope for often come to pass than things we wish.” by Titus Maccius Plautus.
https://finasteride.store/# buying generic propecia no prescription
https://finasteride.store/# cheap propecia without rx
ciprofloxacin generic price buy cipro ciprofloxacin 500mg buy online
lisinopril 20 mg price without prescription: buy lisinopril 20 mg without a prescription – cost of lisinopril 10 mg
http://ciprofloxacin.tech/# ciprofloxacin generic price
lisinopril 2.5 tablet cost of lisinopril 40 mg lisinopril tablets uk
ciprofloxacin 500mg buy online: cipro – ciprofloxacin 500 mg tablet price
http://ciprofloxacin.tech/# ciprofloxacin generic price
Pretty! This was a really wonderful post. Thank you for your provided information.
tamoxifen hip pain tamoxifen bone density tamoxifenworld
http://ciprofloxacin.tech/# buy cipro online
buy generic ciprofloxacin: ciprofloxacin generic price – antibiotics cipro
http://finasteride.store/# buying propecia price
????????-???????, ??? ????? ????? ???????? ??????????? aquanet ???????? ??? ????? ?????? ???????.
http://viagras.online/# Cheapest Sildenafil online
Buy Tadalafil 20mg Generic Tadalafil 20mg price Cialis without a doctor prescription
I love it when people come together and share opinions, great blog, keep it up.
https://cenforce.pro/# order cenforce
???????, ??? ????? ?????? ???????? ???????? ? ??????? ?? ??????? ??????????????.
I take pleasure in, result in I found exactly what I was looking for. You’ve ended my four day lengthy hunt! God Bless you man. Have a nice day. Bye
sildenafil over the counter Cheap Viagra 100mg cheap viagra
super kamagra: kamagra.win – Kamagra 100mg price
https://viagras.online/# buy Viagra over the counter
http://cialist.pro/# Cialis 20mg price
Generic Cialis without a doctor prescription Buy Tadalafil 10mg Generic Cialis without a doctor prescription
https://levitrav.store/# Buy Levitra 20mg online
Cialis over the counter Generic Tadalafil 20mg price cheapest cialis
https://viagras.online/# Viagra generic over the counter
http://levitrav.store/# Levitra generic best price
Generic Tadalafil 20mg price cialist.pro Buy Cialis online
Cheapest Sildenafil online: viagras.online – viagra without prescription
https://kamagra.win/# Kamagra Oral Jelly
Buy Vardenafil 20mg online Vardenafil online prescription Buy Vardenafil 20mg online
http://kamagra.win/# Kamagra 100mg price
cheapest cialis buy cialis overseas Buy Cialis online
http://kamagra.win/# sildenafil oral jelly 100mg kamagra
buy medication online without prescription pharmacy no prescription required best online pharmacy without prescription
https://pharmnoprescription.icu/# no prescription on line pharmacies
canadian pharmacy cheap: trusted canadian pharmacy – online canadian pharmacy
real canadian pharmacy my canadian pharmacy online canadian pharmacy reviews
http://pharmnoprescription.icu/# order prescription from canada
Hello! I just would like to give a huge thumbs up for the great info you have here on this post. I will be coming back to your blog for more soon.
This design is incredible! You certainly know how to keep a reader amused. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Great job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
order prescription from canada: canadian pharmacy no prescription – buying drugs online no prescription
http://pharmcanada.shop/# pharmacy canadian
medication from mexico pharmacy: mexican pharmaceuticals online – ?»?best mexican online pharmacies
canada pharmacy not requiring prescription: pharm world – pharmacy without prescription
medicine in mexico pharmacies purple pharmacy mexico price list pharmacies in mexico that ship to usa
http://pharmworld.store/# mail order pharmacy no prescription
pharmacy coupons: cheapest pharmacy – canadian online pharmacy no prescription
online pharmacy discount code cheapest pharmacy buying prescription drugs from canada
http://pharmnoprescription.icu/# prescription from canada
I really appreciate this post. I have been looking everywhere for this! Thank goodness I found it on Bing. You have made my day! Thx again
mexican rx online mexican mail order pharmacies mexico drug stores pharmacies
http://pharmnoprescription.icu/# mail order prescriptions from canada
????????? ??????????? ???????? ?????? ?????? ? ????? ??????? ???????????, ??????? ?????????? ??? ??????????? ? ????????? ??????????? – https://zakaz-na-diplom.ru. ?????? ????????? ????? ? ?????? ?????????? ? ????????????, ??????????? ??????????? ? ????????????? ??????????? ? ?????????????????? ??????????????. ? ???????? ????????, ??? ??????????? ?? ????? ????? ??? ??????, ??????? ????????? ?????? ??????????? ???????? ??? ???????? ???????????????? ????????????. ?????? ?????????? ???? ??????, ?????? ? ??????, ??????????? ? ?????? ????? ?????????????? ? ????????? ? ?????. ? ??????????, ???????? ?????? ??????????? ? ???? ? ????????? ??????????, ??? ??????????? ????????????? ???????? ? ????????. ?????????? ????? ??????????? ????? ????????? ? ???????, ??????????? ???????????? ? ????????????? ???????? ?????. ??????? ????? ???????? ?????????? ???????? ? ????? ????????? ??????????? ? ?????????? ? ??? ??????????, ????? ??????? ?????? ? ??????? ?? ????? ???????????????? ????????????.
???????? ?? ???? ???????????? ???? ??????????????? ???????, ?? ? ????????????? ???? ??????????????, ??????? ? ???????? ? ????????? ?????. ?? ???????????? ????? ??????????? ?????? ? ?????, ????????? ? ????? ? ?????????????????????. ?????????? ????? ??????? ?????????? ????? ???? ?????? ????????? ??????????, ????? ??????????? ???????? ?? ???????????? ??????????? ? ????????? ??????????. ????? ???? ????????????? ??? ?????? ?????? ? ??????, ??????????? ??? ?????????? ???????????? ? ???????? ????????, ?????? ???????? ? ??????????. ????? ????, ?????????? ????????? ?????????????? ????? ???????????? ? ????????????, ??? ???????? ???? ????????????????? ??? ????????????? ?? ????? ????? ? ????????? ???? ??????????? ? ????????? ???????????? ??? ????????????????? ?????. ????? ???????, ?????????? ????? ????????? ?? ?????? ????????? ???? ?????? ? ???????????????? ????????, ?? ? ?????????? ???? ????? ??????????? ??? ?????????? ????? ? ???????.
mexican border pharmacies shipping to usa: medicine in mexico pharmacies – buying prescription drugs in mexico online
doxycycline tetracycline online doxycycline doxycycline vibramycin
??????? ???????? ???? ??????????? ????????? ? ????????????? ??? ??????????? ????? ????? ??????????? ? ??????? ?? ?????????? ? ?????????? ??????. ??????????? ????????? ????????, ?????????? ? ????????????? ?????? ? ??????? ?? ????? ?????????. ?????? ? ??????? ?? ?????????? ?? ?????? ??????? ??? ????????? ????????? ?????, ?? ? ??????? ????????? ?????????? ????? ?? ????. ??????????? ????????? ???????? ?? ?????????? ? ???????? ?????????????? ?????? ????????. ????????? ????? https://serialy-na-angliiskom.pp.ua.
Sweet web site, super design, really clean and use genial.
https://doxycyclinea.online/# 200 mg doxycycline
buy cheap generic zithromax: generic zithromax 500mg – zithromax purchase online
prednisone 30 mg daily: brand prednisone – purchase prednisone 10mg
400 mg prednisone prednisone 80 mg daily otc prednisone cream
prednisone best prices: prednisone 10mg tablet cost – prednisone 10 mg tablet
Great V I should certainly pronounce, impressed with your web site. I had no trouble navigating through all tabs and related info ended up being truly easy to do to access. I recently found what I hoped for before you know it at all. Quite unusual. Is likely to appreciate it for those who add forums or anything, website theme . a tones way for your client to communicate. Nice task..
http://zithromaxa.store/# zithromax tablets
You actually make it seem so easy with your presentation but I find this topic to be actually something that I think I would never understand. It seems too complicated and extremely broad for me. I am looking forward for your next post, I will try to get the hang of it!
how to get zithromax over the counter: zithromax online – can i buy zithromax over the counter
zithromax buy online: zithromax cost – zithromax 250 mg pill
I was wondering if you ever thought of changing the structure of your blog? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
prednisone 5 mg tablet without a prescription: prednisone 1mg purchase – can you buy prednisone online uk
Wow! Thank you! I permanently wanted to write on my website something like that. Can I take a part of your post to my website?
prednisone online sale: prednisone – buy prednisone mexico
neurontin tablets 300 mg neurontin buy online neurontin 400mg
Hi!
Unlock the potential of your finances with binary options trading on our platform! Our platform offers a simple, fast and secure way to invest and earn returns of up to 200% with minimal risk. With a minimum deposit of just $10, you can start your trading journey and see your profits grow in no time.
Earn every minute without limit of $100, $500, $1,000, with a minimum bet of $1.
Instant withdrawal!!!
Bonus code: OLYMPOLYMP
From $50 +30% to deposit!
+ Demo account!
+ Free Signals!
WARNING! If you are trying to access the site from the following countries, you need to enable VPN which does not apply to the following countries!
Australia, Canada, USA, Japan, UK, EU (all countries), Israel, Russia, Iran, Iraq, Korea, Central African Republic, Congo, Cote d’Ivoire, Eritrea, Ethiopia, Lebanon, Liberia, Libya, Mali, Mauritius, Myanmar, New Zealand, Saint Vincent and the Grenadines, Somalia, Sudan, Syria, Vanuatu, Yemen, Zimbabwe.
Sign up and start earning from the first minute!
https://trkmad.com/101773
generic zithromax online paypal: where can you buy zithromax – how much is zithromax 250 mg
zithromax 600 mg tablets buy zithromax without presc zithromax 500 tablet
Hi!
Take your financial future into your own hands with binary options trading! Our platform offers fast and secure trades, with returns up to 800%. Start your investment journey today with just $10.
Earn every minute without limit of $100, $500, $1,000, with a minimum bet of $1.
Instant withdrawal!!!
Bonus code: OLYMPOLYMP
From $50 +30% to deposit!
+ Demo account!
+ Free Signals!
WARNING! If you are trying to access the site from the following countries, you need to enable VPN which does not apply to the following countries!
Australia, Canada, USA, Japan, UK, EU (all countries), Israel, Russia, Iran, Iraq, Korea, Central African Republic, Congo, Cote d’Ivoire, Eritrea, Ethiopia, Lebanon, Liberia, Libya, Mali, Mauritius, Myanmar, New Zealand, Saint Vincent and the Grenadines, Somalia, Sudan, Syria, Vanuatu, Yemen, Zimbabwe.
Sign up and start earning from the first minute!
https://trkmad.com/101773
doxycycline 50mg: doxylin – doxycycline order online
buy cheap doxycycline: doxycycline pills – order doxycycline
???????? ??? ??????????? ????? ? ??????? ??????????! ?? ????? ????? ?? ??????? ?????? ???????? ??? ???? ?????: ???????????, ?????????? ?????????? ??????, ???????? ????????, ?????, ???????? ????????, ?????????? ? ??????? ???????. ?????? [url=https://uchebniki-anglijskogo-yazyka.pp.ua/]https://uchebniki-anglijskogo-yazyka.pp.ua/[/url] ? ??????? ??????????? ???????? ??????????? ????? ????? ??????!
http://prednisoned.online/# how to buy prednisone
neurontin 300 mg coupon neurontin 50 mg neurontin 100 mg caps
you’re really a good webmaster. The site loading speed is incredible. It seems that you are doing any unique trick. In addition, The contents are masterpiece. you have done a great job on this topic!
prescription drug neurontin: neurontin mexico – medicine neurontin 300 mg
buy zithromax without prescription online: can you buy zithromax over the counter in canada – zithromax tablets
http://doxycyclinea.online/# buy doxycycline online
amoxicillin buy canada buy amoxicillin online cheap buy amoxicillin online with paypal
Hi!
Elevate your investment game with binary options trading on our platform. Earn returns up to 200% with a low $10 deposit. Trade with ease using real-time market analysis and a user-friendly interface. Stay in control with anytime, anywhere access and top-notch security measures. Start your successful trading journey now!
Earn every minute without limit of $100, $500, $1,000, with a minimum bet of $1.
Instant withdrawal!!!
Bonus code: OLYMPOLYMP
From $50 +30% to deposit!
+ Demo account!
+ Free Signals!
WARNING! If you are trying to access the site from the following countries, you need to enable VPN which does not apply to the following countries!
Australia, Canada, USA, Japan, UK, EU (all countries), Israel, Russia, Iran, Iraq, Korea, Central African Republic, Congo, Cote d’Ivoire, Eritrea, Ethiopia, Lebanon, Liberia, Libya, Mali, Mauritius, Myanmar, New Zealand, Saint Vincent and the Grenadines, Somalia, Sudan, Syria, Vanuatu, Yemen, Zimbabwe.
Sign up and start earning from the first minute!
https://trkmad.com/101773
zithromax prescription in canada: zithromax over the counter – zithromax buy
prednisone 20mg by mail order prednisone where can i buy prednisone cost 10mg
http://prednisoned.online/# buy prednisone from canada
I truly appreciate this post. I?¦ve been looking everywhere for this! Thank goodness I found it on Bing. You’ve made my day! Thanks again
Hi!
Our platform provides real-time market analysis and updates to help guide your decisions, making the trading process effortless and stress-free. Whether you prefer to trade on-the-go or from the comfort of your own home, our platform is accessible from anywhere with an internet connection. You can trade with confidence knowing that our platform has the highest level of security measures in place to protect your funds.
Earn every minute without limit of $100, $500, $1,000, with a minimum bet of $1.
Instant withdrawal!!!
Bonus code: OLYMPOLYMP
From $50 +30% to deposit!
+ Demo account!
+ Free Signals!
WARNING! If you are trying to access the site from the following countries, you need to enable VPN which does not apply to the following countries!
Australia, Canada, USA, Japan, UK, EU (all countries), Israel, Russia, Iran, Iraq, Korea, Central African Republic, Congo, Cote d’Ivoire, Eritrea, Ethiopia, Lebanon, Liberia, Libya, Mali, Mauritius, Myanmar, New Zealand, Saint Vincent and the Grenadines, Somalia, Sudan, Syria, Vanuatu, Yemen, Zimbabwe.
Sign up and start earning from the first minute!
https://trkmad.com/101773
zithromax capsules price: cost of generic zithromax – buy zithromax no prescription
generic amoxicillin cost: amoxicillin 500mg no prescription – how to get amoxicillin
prescription prednisone cost buy prednisone without a prescription prednisone 20mg online
http://doxycyclinea.online/# doxycycline hyc
generic for doxycycline: online doxycycline – doxycycline
buy cheap zithromax online: zithromax online usa – zithromax online
Hi!
Unleash the potential of your money with binary options trading! Our platform offers fast and secure trades, with a range of assets to choose from and returns up to 800%. Start your journey to financial freedom with just $10.
Earn every minute without limit of $100, $500, $1,000, with a minimum bet of $1.
Instant withdrawal!!!
Bonus code: OLYMPOLYMP
From $50 +30% to deposit!
+ Demo account!
+ Free Signals!
WARNING! If you are trying to access the site from the following countries, you need to enable VPN which does not apply to the following countries!
Australia, Canada, USA, Japan, UK, EU (all countries), Israel, Russia, Iran, Iraq, Korea, Central African Republic, Congo, Cote d’Ivoire, Eritrea, Ethiopia, Lebanon, Liberia, Libya, Mali, Mauritius, Myanmar, New Zealand, Saint Vincent and the Grenadines, Somalia, Sudan, Syria, Vanuatu, Yemen, Zimbabwe.
Sign up and start earning from the first minute!
https://trkmad.com/101773
where can i get doxycycline doxycycline 100mg buy doxycycline without prescription
http://amoxila.pro/# can i buy amoxicillin online
F*ckin’ awesome things here. I am very glad to see your article. Thanks a lot and i am looking forward to touch you. Will you please drop me a mail?
neurontin prescription online: neurontin 300mg – neurontin mexico
generic zithromax online paypal can i buy zithromax online buy zithromax online fast shipping
zithromax 1000 mg pills: zithromax 500 mg – zithromax buy online
Hi!
Join the thousands of traders making big profits with binary options trading! Our user-friendly platform offers fast trades, secure transactions, and returns as high as 900%. Start with a minimum deposit of just $10.
Earn every minute without limit of $100, $500, $1,000, with a minimum bet of $1.
Instant withdrawal!!!
Bonus code: OLYMPOLYMP
From $50 +30% to deposit!
+ Demo account!
+ Free Signals!
WARNING! If you are trying to access the site from the following countries, you need to enable VPN which does not apply to the following countries!
Australia, Canada, USA, Japan, UK, EU (all countries), Israel, Russia, Iran, Iraq, Korea, Central African Republic, Congo, Cote d’Ivoire, Eritrea, Ethiopia, Lebanon, Liberia, Libya, Mali, Mauritius, Myanmar, New Zealand, Saint Vincent and the Grenadines, Somalia, Sudan, Syria, Vanuatu, Yemen, Zimbabwe.
Sign up and start earning from the first minute!
https://trkmad.com/101773
https://doxycyclinea.online/# doxycycline hydrochloride 100mg
doxycycline 100mg price: buy doxycycline online – order doxycycline
amoxicillin 500mg capsule buy online amoxicillin 500 mg capsule generic amoxicillin over the counter
https://prednisoned.online/# can you buy prednisone
neurontin 400 mg capsule: neurontin 800 – neurontin prices generic
It’s appropriate time to make a few plans for the future and it is time to be happy. I have learn this publish and if I could I wish to recommend you few attention-grabbing issues or advice. Maybe you could write next articles referring to this article. I want to learn even more things approximately it!
buy zithromax online cheap zithromax 500mg price in india zithromax 500 price
http://gabapentinneurontin.pro/# order neurontin
I’ve recently started a site, the information you offer on this website has helped me tremendously. Thank you for all of your time & work. “The achievements of an organization are the results of the combined effort of each individual.” by Vince Lombardi.
Hi!
Take control of your finances with binary options trading on our platform. Earn returns up to 200% with a minimum deposit of just $10. Simple, fast and secure trading with real-time market analysis. Trade from anywhere, at any time, with our user-friendly interface and top-notch security measures. Join the successful traders on our platform today!
Earn every minute without limit of $100, $500, $1,000, with a minimum bet of $1.
Instant withdrawal!!!
Bonus code: OLYMPOLYMP
From $50 +30% to deposit!
+ Demo account!
+ Free Signals!
WARNING! If you are trying to access the site from the following countries, you need to enable VPN which does not apply to the following countries!
Australia, Canada, USA, Japan, UK, EU (all countries), Israel, Russia, Iran, Iraq, Korea, Central African Republic, Congo, Cote d’Ivoire, Eritrea, Ethiopia, Lebanon, Liberia, Libya, Mali, Mauritius, Myanmar, New Zealand, Saint Vincent and the Grenadines, Somalia, Sudan, Syria, Vanuatu, Yemen, Zimbabwe.
Sign up and start earning from the first minute!
https://trkmad.com/101773
buy neurontin online: neurontin prescription – neurontin 300 mg cap
Hey, you used to write fantastic, but the last few posts have been kinda boring… I miss your great writings. Past few posts are just a little bit out of track! come on!
amoxicillin where to get: amoxicillin online canada – amoxicillin 500mg tablets price in india
can you buy zithromax over the counter buy zithromax online cheap zithromax 500 tablet
http://prednisoned.online/# prednisone 50 mg tablet cost
I am often to blogging and i really appreciate your content. The article has really peaks my interest. I am going to bookmark your site and keep checking for new information.
I’ve recently started a website, the info you provide on this website has helped me greatly. Thanks for all of your time & work.
generic doxycycline: doxycycline hyclate 100 mg cap – doxycycline 100mg online
generic neurontin pill: neurontin prices – purchase neurontin online
order zithromax over the counter buy zithromax online with mastercard cheap zithromax pills
http://doxycyclinea.online/# buy doxycycline without prescription uk
order doxycycline: buy doxycycline for dogs – buy doxycycline hyclate 100mg without a rx
odering doxycycline: buy cheap doxycycline – doxycycline 100mg tablets
how much is prednisone 10mg prednisone 10 tablet prednisone 0.5 mg
https://doxycyclinea.online/# buy cheap doxycycline
zithromax coupon: zithromax 500 tablet – buy zithromax 1000 mg online
buy doxycycline 100mg: doxycycline 100mg price – cheap doxycycline online
buy zithromax online australia zithromax 250 mg zithromax price canada
Magnificent website. Plenty of useful information here. I’m sending it to several friends ans additionally sharing in delicious. And certainly, thank you for your effort!
Awsome blog! I am loving it!! Will come back again. I am bookmarking your feeds also.
https://amoxila.pro/# buy amoxicillin without prescription
https://mexicanpharmacy1st.com/# medication from mexico pharmacy
purple pharmacy mexico price list pharmacies in mexico that ship to usa buying from online mexican pharmacy
https://mexicanpharmacy1st.shop/# mexican online pharmacies prescription drugs
buying prescription drugs in mexico: purple pharmacy mexico price list – reputable mexican pharmacies online
mexico drug stores pharmacies: mexico drug stores pharmacies – medication from mexico pharmacy
?»?best mexican online pharmacies buying from online mexican pharmacy ?»?best mexican online pharmacies
mexican online pharmacies prescription drugs: mexican rx online – ?»?best mexican online pharmacies
I’ve been absent for some time, but now I remember why I used to love this blog. Thank you, I’ll try and check back more frequently. How frequently you update your site?
https://mexicanpharmacy1st.online/# buying prescription drugs in mexico
pharmacies in mexico that ship to usa medication from mexico pharmacy reputable mexican pharmacies online
??????? ???????? ???? ??????????? ??????????? ? ????????????? ??? ??????????? ????? ????? ?????????? ? ??????? ?? ??????????. ??????????? ????????? ????????, ?????????? ? ??????????? ?????? ? ??????? ?? ????? ?????????. ????????? ?? ????? https://serialy-na-angliiskom.pp.ua. ?????? ? ??????? ?? ?????????? ?? ?????? ??????? ??? ????????? ????????? ?????, ?? ? ??????? ????????? ?????????? ????? ?? ????. ??????????? ????????? ???????? ?? ?????????? ? ???????? ?????????????? ?????? ????????.
mexican drugstore online: mexican pharmacy – mexican mail order pharmacies
As I website owner I think the content here is real wonderful, thankyou for your efforts.
https://mexicanpharmacy1st.com/# mexico pharmacies prescription drugs
mexico pharmacies prescription drugs mexico drug stores pharmacies reputable mexican pharmacies online
https://mexicanpharmacy1st.online/# mexico pharmacy
The next time I read a blog, I hope that it doesnt disappoint me as much as this one. I mean, I know it was my choice to read, but I actually thought youd have something interesting to say. All I hear is a bunch of whining about something that you could fix if you werent too busy looking for attention.
pharmacies in mexico that ship to usa: reputable mexican pharmacies online – purple pharmacy mexico price list
purple pharmacy mexico price list: purple pharmacy mexico price list – mexican border pharmacies shipping to usa
https://mexicanpharmacy1st.com/# mexico pharmacies prescription drugs
mexico pharmacy buying prescription drugs in mexico online best online pharmacies in mexico
mexican border pharmacies shipping to usa: buying prescription drugs in mexico – medication from mexico pharmacy
mexican pharmaceuticals online: buying prescription drugs in mexico – mexico drug stores pharmacies
https://mexicanpharmacy1st.com/# best online pharmacies in mexico
buying prescription drugs in mexico mexican online pharmacies prescription drugs ?»?best mexican online pharmacies
medication from mexico pharmacy: mexico drug stores pharmacies – mexico drug stores pharmacies
Great post but I was wanting to know if you could write a litte more on this subject? I’d be very grateful if you could elaborate a little bit further. Kudos!
https://mexicanpharmacy1st.shop/# buying from online mexican pharmacy
mexican online pharmacies prescription drugs buying prescription drugs in mexico online buying from online mexican pharmacy
mexico pharmacies prescription drugs: mexican rx online – purple pharmacy mexico price list
mexican pharmaceuticals online: mexico pharmacy – reputable mexican pharmacies online
http://mexicanpharmacy1st.com/# mexican online pharmacies prescription drugs
reputable mexican pharmacies online mexican pharmacy buying prescription drugs in mexico
https://mexicanpharmacy1st.com/# purple pharmacy mexico price list
buying prescription drugs in mexico online: pharmacies in mexico that ship to usa – best mexican online pharmacies
lisinopril 2.5 mg medicine: prinivil coupon – lisinopril 20 mg tab price
where can i get cheap clomid price: how can i get cheap clomid price – can you get clomid pills
how can i get cheap clomid without prescription generic clomid pill get clomid without a prescription
cost generic propecia no prescription: cost generic propecia without prescription – order generic propecia
lisinopril 40 mg mexico lisinopril 250 mg lisinopril 2.5 mg buy online
lisinopril 4214 zestoretic 20 25 mg lisinopril 3973
10mg generic 10mg lisinopril: lisinopril tabs 10mg – lisinopril 20 mg discount
Hiya very cool blog!! Man .. Excellent .. Superb .. I’ll bookmark your website and take the feeds also…I am happy to find so many helpful info here within the submit, we need develop extra techniques in this regard, thanks for sharing.
https://propeciaf.online/# cost of propecia
propecia without insurance: order generic propecia no prescription – propecia without a prescription
buy generic propecia no prescription cost of generic propecia tablets order generic propecia no prescription
order cytotec online: cytotec pills buy online – ?»?cytotec pills online
buy cytotec over the counter: buy cytotec pills online cheap – Cytotec 200mcg price
https://clomiphene.shop/# how to get clomid no prescription
Abortion pills online order cytotec online ?»?cytotec pills online
neurontin cost uk: neurontin 600 mg tablet – generic gabapentin
I like the helpful info you provide in your articles. I’ll bookmark your weblog and check again here regularly. I am quite sure I’ll learn many new stuff right here! Good luck for the next!
I?¦m no longer certain the place you’re getting your info, however great topic. I needs to spend some time studying much more or understanding more. Thanks for fantastic information I used to be searching for this information for my mission.
order cytotec online buy cytotec online cytotec buy online usa
This is a very good tips especially to those new to blogosphere, brief and accurate information… Thanks for sharing this one. A must read article.
buy cytotec in usa: Cytotec 200mcg price – cytotec buy online usa
I would like to thnkx for the efforts you have put in writing this blog. I am hoping the same high-grade blog post from you in the upcoming as well. In fact your creative writing abilities has inspired me to get my own blog now. Really the blogging is spreading its wings quickly. Your write up is a good example of it.
lisinopril 40 mg brand name in india: buy cheap lisinopril 40mg – where can i get lisinopril
http://propeciaf.online/# cost cheap propecia without prescription
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get several e-mails with the
same comment. Is there any way you can remove me from that service?
Thank you!
My site … facebook vs eharmony to find love online
buy cytotec order cytotec online purchase cytotec
buy cytotec pills online cheap: cytotec abortion pill – order cytotec online
canadian pharmacy 365 precription drugs from canada canada pharmacy online
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You definitely know what youre talking about, why throw away your intelligence on just posting videos to your weblog when you could be giving us something informative to read?
https://36and6health.shop/# buying prescription drugs from canada
I’ve been exploring for a bit for any high quality articles or blog posts on this kind of area . Exploring in Yahoo I at last stumbled upon this website. Reading this info So i am happy to convey that I have an incredibly good uncanny feeling I discovered exactly what I needed. I most certainly will make sure to do not forget this web site and give it a look regularly.
Regards for this post, I am a big big fan of this website would like to proceed updated.
https://cheapestandfast.shop/# online meds without prescription
Precisely what I was searching for, thankyou for putting up.
ordering drugs from canada canadian pharmacy near me vipps approved canadian online pharmacy
Wow! Thank you! I always wanted to write on my blog something like that. Can I implement a part of your post to my blog?
https://cheapestindia.shop/# mail order pharmacy india
Hey, you used to write great, but the last few posts have been kinda boringK I miss your super writings. Past few posts are just a little out of track! come on!
I always was interested in this topic and stock still am, thankyou for posting.
http://cheapestandfast.com/# buy medications without prescriptions
Thank you for sharing with us, I believe this website genuinely stands out : D.
https://cheapestindia.com/# india pharmacy
Neat blog! Is your theme custom made or did you download it from somewhere? A design like yours with a few simple adjustements would really make my blog stand out. Please let me know where you got your theme. With thanks
Hmm is anyone else having problems with the pictures on this blog loading? I’m trying to find out if its a problem on my end or if it’s the blog. Any suggestions would be greatly appreciated.
Having read this I thought it was very informative. I appreciate you taking the time and effort to put this article together. I once again find myself spending way to much time both reading and commenting. But so what, it was still worth it!
I have read a few good stuff here. Definitely price bookmarking for revisiting. I surprise how a lot effort you set to create such a great informative site.
After all, what a great site and informative posts, I will upload inbound link – bookmark this web site? Regards, Reader.
indian pharmacy paypal indian pharmacy paypal Online medicine order
https://cheapestcanada.com/# vipps canadian pharmacy
https://cheapestmexico.shop/# mexican drugstore online
https://cheapestmexico.com/# mexico pharmacy
Thanks for sharing superb informations. Your web-site is very cool. I am impressed by the details that you’ve on this blog. It reveals how nicely you understand this subject. Bookmarked this website page, will come back for more articles. You, my pal, ROCK! I found simply the info I already searched everywhere and simply could not come across. What an ideal web site.
vente de m?©dicament en ligne acheter m?©dicament en ligne sans ordonnance ?»?pharmacie en ligne france
Pharmacie en ligne livraison Europe: Pharmacie sans ordonnance – pharmacie en ligne france livraison internationale
pharmacie en ligne france livraison internationale: trouver un m̩dicament en pharmacie РPharmacie Internationale en ligne
http://eufarmacieonline.com/# Farmacia online miglior prezzo
online apotheke versandkostenfrei g??nstigste online apotheke ?»?shop apotheke gutschein
farmacia en casa online descuento: farmacias online seguras – farmacias online seguras en espa?±a
?»?pharmacie en ligne france: pharmacies en ligne certifi?©es – Pharmacie sans ordonnance
apotheke online: online apotheke rezept – shop apotheke gutschein
Farmacie online sicure: Farmacie online sicure – farmacia online
pharmacies en ligne certifi?©es pharmacie en ligne fiable vente de m?©dicament en ligne
farmacia online env?o gratis: farmacias online seguras – farmacia online 24 horas
online apotheke: beste online-apotheke ohne rezept – apotheke online
farmacia online barcelona: farmacia online 24 horas – farmacias online seguras
https://euapothekeohnerezept.shop/# medikamente rezeptfrei
pharmacie en ligne sans ordonnance: acheter m̩dicament en ligne sans ordonnance Рpharmacie en ligne livraison europe
online apotheke versandkostenfrei internet apotheke beste online-apotheke ohne rezept
farmacias online seguras en espa?±a: farmacia online barcelona – farmacia online barata y fiable
comprare farmaci online con ricetta: farmacia online – acquisto farmaci con ricetta
farmacias online seguras: farmacias direct – farmacia online barata
farmacias online seguras en espa?±a farmacia online espa?±a env?o internacional farmacias online seguras en espa?±a
pharmacie en ligne fiable: pharmacie en ligne france livraison internationale – Pharmacie Internationale en ligne
http://euapothekeohnerezept.com/# online apotheke g??nstig
farmacia online 24 horas farmacia online madrid farmacia barata
I used to be suggested this web site through my cousin. I’m no longer sure whether or not this post is written by means of him as no one else recognize such distinctive approximately my difficulty. You are wonderful! Thanks!
farmacias online seguras en espa?±a: farmacia barata – farmacia online barata
comprare farmaci online all’estero: farmaci senza ricetta elenco – farmacie online affidabili
This blog is definitely rather handy since I’m at the moment creating an internet floral website – although I am only starting out therefore it’s really fairly small, nothing like this site. Can link to a few of the posts here as they are quite. Thanks much. Zoey Olsen
farmacias direct farmacias online baratas farmacia en casa online descuento
farmacia online pi?? conveniente: Farmacia online pi?? conveniente – farmacie online sicure
comprare farmaci online all’estero: Farmacia online migliore – Farmacia online più conveniente
Farmacia online pi?? conveniente: comprare farmaci online all’estero – migliori farmacie online 2024
farmacia online senza ricetta: Farmacie on line spedizione gratuita – comprare farmaci online con ricetta
https://euapothekeohnerezept.shop/# eu apotheke ohne rezept
trouver un m?©dicament en pharmacie: levitra generique prix en pharmacie – pharmacie en ligne fiable
Thank you for any other informative website. Where else may I am getting that type of information written in such an ideal manner? I’ve a venture that I’m simply now operating on, and I have been on the glance out for such information.
vente de m?©dicament en ligne: achat kamagra – Pharmacie sans ordonnance
trouver un m?©dicament en pharmacie: pharmacie en ligne sans ordonnance – pharmacie en ligne france livraison internationale
Sweet web site, super pattern, very clean and apply pleasant.
?»?pharmacie en ligne france: kamagra gel – trouver un m?©dicament en pharmacie
pharmacies en ligne certifi?©es: Acheter Cialis 20 mg pas cher – pharmacie en ligne avec ordonnance
trouver un m?©dicament en pharmacie: cialis prix – pharmacie en ligne france livraison internationale
You have brought up a very good points, thankyou for the post.
Viagra pas cher livraison rapide france: Viagra vente libre pays – Viagra vente libre allemagne
pharmacie en ligne avec ordonnance: kamagra 100mg prix – Achat m?©dicament en ligne fiable
Hello!
This post was created with XRumer 23 StrongAI.
Good luck 🙂
pharmacie en ligne sans ordonnance: Acheter Cialis – trouver un m?©dicament en pharmacie
trouver un m?©dicament en pharmacie: Levitra acheter – Pharmacie sans ordonnance
Pharmacie sans ordonnance: Pharmacie en ligne livraison Europe – vente de m?©dicament en ligne
Achat m?©dicament en ligne fiable: kamagra pas cher – trouver un m?©dicament en pharmacie
https://kamagraenligne.shop/# trouver un médicament en pharmacie
?»?pharmacie en ligne france: Levitra sans ordonnance 24h – vente de m?©dicament en ligne
vente de m?©dicament en ligne: Levitra sans ordonnance 24h – pharmacie en ligne pas cher
Hello.
This post was created with XRumer 23 StrongAI.
Good luck 🙂
pharmacie en ligne france livraison internationale: Levitra acheter – ?»?pharmacie en ligne france
?»?pharmacie en ligne france: Pharmacie Internationale en ligne – pharmacies en ligne certifi?©es
Hello very nice website!! Guy .. Beautiful .. Superb .. I’ll bookmark your web site and take the feeds also…I am glad to find a lot of useful info right here in the post, we’d like develop more techniques on this regard, thanks for sharing. . . . . .
When I originally commented I clicked the -Notify me when new comments are added- checkbox and now each time a comment is added I get four emails with the same comment. Is there any way you can remove me from that service? Thanks!
pharmacie en ligne france pas cher: kamagra pas cher – pharmacie en ligne pas cher
Fine way of telling, and good paragraph to take information about my presentation subject matter, which
i am going to convey in college.
Feel free to visit my site eharmony special coupon code 2024
You actually make it seem really easy along with your presentation but I to find this topic to be really something which I think I would by no means understand. It sort of feels too complicated and extremely vast for me. I’m looking ahead in your subsequent post, I¦ll try to get the cling of it!
pharmacie en ligne livraison europe: Medicaments en ligne livres en 24h – Pharmacie Internationale en ligne
pharmacie en ligne: Acheter Cialis 20 mg pas cher – pharmacie en ligne avec ordonnance
pharmacie en ligne: kamagra en ligne – Pharmacie Internationale en ligne
pharmacie en ligne france fiable: pharmacie en ligne – pharmacie en ligne sans ordonnance
Some genuinely superb info , Gladiolus I observed this.
pharmacie en ligne france pas cher: pharmacie en ligne sans ordonnance – pharmacie en ligne france fiable
pharmacie en ligne sans ordonnance: pharmacie en ligne pas cher – Pharmacie Internationale en ligne
Achat m?©dicament en ligne fiable: Pharmacies en ligne certifiees – acheter m?©dicament en ligne sans ordonnance
Viagra homme prix en pharmacie sans ordonnance: viagra sans ordonnance – Viagra pas cher inde
pharmacie en ligne france pas cher: trouver un m?©dicament en pharmacie – pharmacie en ligne fiable
Acheter Sildenafil 100mg sans ordonnance: Meilleur Viagra sans ordonnance 24h – Sildenafil teva 100 mg sans ordonnance
I haven¦t checked in here for some time because I thought it was getting boring, but the last few posts are good quality so I guess I will add you back to my daily bloglist. You deserve it my friend 🙂
Pharmacie en ligne livraison Europe: kamagra gel – pharmacies en ligne certifi?©es
It’s really a great and helpful piece of information. I’m glad that you shared this helpful information with us. Please keep us informed like this. Thanks for sharing.
pharmacie en ligne france fiable: pharmacie en ligne fiable – pharmacie en ligne fiable
Viagra vente libre pays: Viagra 100 mg sans ordonnance – Sild?©nafil Teva 100 mg acheter
very nice put up, i actually love this website, carry on it
Pharmacie sans ordonnance: kamagra en ligne – pharmacie en ligne pas cher
pharmacie en ligne france fiable: Acheter Cialis – pharmacie en ligne france fiable
I would like to thnkx for the efforts you have put in writing this blog. I am hoping the same high-grade blog post from you in the upcoming as well. In fact your creative writing abilities has inspired me to get my own blog now. Really the blogging is spreading its wings quickly. Your write up is a good example of it.
pharmacie en ligne avec ordonnance: cialis generique – acheter m?©dicament en ligne sans ordonnance
?»?pharmacie en ligne france: achat kamagra – pharmacie en ligne livraison europe
pharmacie en ligne france livraison internationale: Levitra pharmacie en ligne – trouver un m?©dicament en pharmacie
very good put up, i definitely love this web site, carry on it
pharmacie en ligne france livraison belgique: Acheter Cialis – Pharmacie Internationale en ligne
I’m really inspired together with your writing abilities and also with the structure for your weblog. Is that this a paid topic or did you customize it your self? Either way keep up the excellent quality writing, it is rare to peer a great weblog like this one today..
I have not checked in here for some time as I thought it was getting boring, but the last several posts are great quality so I guess I?¦ll add you back to my daily bloglist. You deserve it my friend 🙂
You really make it seem so easy with your presentation but I find this topic to be actually something which I think I would never understand. It seems too complicated and very broad for me. I am looking forward for your next post, I will try to get the hang of it!
It’s hard to find knowledgeable people on this topic, but you sound like you know what you’re talking about! Thanks
For newest information you have to visit internet and
on the web I found this web page as a most excellent website for hottest updates.
Yeah bookmaking this wasn’t a speculative conclusion outstanding post! .
Hey there! I just wanted to ask if you ever have any problems with hackers? My last blog (wordpress) was hacked and I ended up losing several weeks of hard work due to no backup. Do you have any solutions to prevent hackers?
Everything is very open and very clear explanation of issues. was truly information. Your website is very useful. Thanks for sharing.
Generally I don’t read article on blogs, however I would like to say that this write-up very forced me to take a look at and do so! Your writing style has been amazed me. Thanks, very nice post.
Hello, you used to write fantastic, but the last several posts have been kinda boring?K I miss your super writings. Past few posts are just a bit out of track! come on!
Some genuinely good content on this site, thank you for contribution. “Such evil deeds could religion prompt.” by Lucretius.
What Is FitSpresso? FitSpresso is a dietary supplement that is made to support healthy fat-burning in the body
Pretty nice post. I just stumbled upon your blog and wanted to say that I’ve really enjoyed surfing around your blog posts. After all I’ll be subscribing to your rss feed and I hope you write again very soon!
I?¦ll immediately snatch your rss feed as I can’t to find your email subscription link or e-newsletter service. Do you have any? Please let me recognize so that I may just subscribe. Thanks.
Just want to say your article is as astounding. The clearness in your post is just spectacular and i can assume you are an expert on this subject. Fine with your permission allow me to grab your RSS feed to keep up to date with forthcoming post. Thanks a million and please continue the rewarding work.
I just couldn’t depart your website before suggesting that I extremely enjoyed the standard information a person provide for your visitors? Is gonna be back often in order to check up on new posts
You really make it seem really easy together with your presentation however I find this matter to be really one thing that I believe I might by no means understand. It kind of feels too complex and extremely vast for me. I am taking a look ahead on your next publish, I¦ll attempt to get the grasp of it!
Thanks for every other fantastic post. Where else could anybody get that type of info in such a perfect means of writing? I’ve a presentation next week, and I’m on the search for such info.
Some truly choice blog posts on this web site, saved to favorites.
You have brought up a very fantastic details, appreciate it for the post.
Generally I don’t learn article on blogs, but I wish to say that this write-up very pressured me to take a look at and do it! Your writing taste has been amazed me. Thanks, quite nice article.
I like this blog so much, saved to my bookmarks.
But wanna state that this is handy, Thanks for taking your time to write this.
Usually I do not learn article on blogs, however I would like to say that this write-up very pressured me to take a look at and do it! Your writing taste has been surprised me. Thank you, very great post.
Good day! Do you know if they make any plugins to help with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good success. If you know of any please share. Appreciate it!
Hi my loved one! I wish to say that this article is amazing, great written and come with almost all important infos. I would like to look more posts like this .
Hiya! I just would like to give an enormous thumbs up for the good information you might have here on this post. I will be coming back to your weblog for more soon.
????? ???? ? ????? ?????
?????? ?????? ??????????? ???????????? ??????????? ????? ??? ???????
I like this site very much, Its a real nice situation to read and find info .
I’m writing to let you be aware of what a impressive encounter my cousin’s daughter obtained going through your blog. She came to understand numerous pieces, with the inclusion of how it is like to have a marvelous teaching style to get the mediocre ones completely know just exactly a variety of advanced issues. You truly surpassed her expected results. Thank you for providing the productive, healthy, revealing and also fun tips about that topic to Lizeth.
Merely wanna remark that you have a very decent site, I enjoy the design it really stands out.
It’s hard to find knowledgeable folks on this subject, however you sound like you understand what you’re speaking about! Thanks
This is really interesting, You are a very skilled blogger. I have joined your rss feed and look forward to seeking more of your fantastic post. Also, I have shared your web site in my social networks!
There are definitely quite a lot of details like that to take into consideration. That is a nice point to bring up. I provide the thoughts above as normal inspiration however clearly there are questions like the one you deliver up the place an important thing will likely be working in honest good faith. I don?t know if best practices have emerged around issues like that, however I am sure that your job is clearly identified as a fair game. Both girls and boys really feel the affect of just a second’s pleasure, for the rest of their lives.
obviously like your website however you have to check the spelling on several of your posts. A number of them are rife with spelling issues and I to find it very bothersome to inform the reality nevertheless I¦ll surely come again again.
I will right away grab your rss as I can’t find your e-mail subscription link or newsletter service. Do you have any? Please let me know so that I could subscribe. Thanks.
I am sure this article has touched all the internet viewers, its really really fastidious post on building up new webpage.
Hello There. I found your blog using msn. This is a really well
written article. I’ll make sure to bookmark it and come back to
read more of your useful information. Thanks for
the post. I’ll certainly comeback.
Somebody necessarily assist to make severely articles I would state.
That is the very first time I frequented your website page and thus far?
I surprised with the research you made to create this particular put up incredible.
Excellent activity!
Oh my goodness! Incredible article dude! Thank you, However
I am encountering troubles with your RSS. I don’t
know the reason why I cannot subscribe to it.
Is there anyone else having the same RSS
issues? Anybody who knows the solution can you kindly respond?
Thanks!!
I like this website so much, saved to favorites. “To hold a pen is to be at war.” by Francois Marie Arouet Voltaire.
That is very interesting, You are an overly professional blogger.
I have joined your feed and sit up for searching for extra of your wonderful
post. Additionally, I’ve shared your website in my social networks
I’m amazed, I must say. Rarely do I encounter a blog that’s both educative
and engaging, and let me tell you, you have hit the nail on the
head. The problem is something that not enough folks are speaking intelligently about.
Now i’m very happy that I found this during my search for something
relating to this.
Hey there! I just wanted to ask if you ever have any trouble with hackers?
My last blog (wordpress) was hacked and I ended up losing months of hard
work due to no backup. Do you have any methods to protect against hackers?
Hey there! I know this is kind of off topic but I was wondering if you
knew where I could get a captcha plugin for
my comment form? I’m using the same blog platform as yours and I’m having
problems finding one? Thanks a lot!
Great write-up, I¦m regular visitor of one¦s blog, maintain up the nice operate, and It is going to be a regular visitor for a lengthy time.
Article writing is also a fun, if you know afterward
you can write otherwise it is complicated to write.
I enjoy looking through an article that can make men and women think.
Also, many thanks for allowing me to comment!
I am not sure where you’re getting your info,
but great topic. I needs to spend some time learning much more or understanding more.
Thanks for magnificent info I was looking for this information for my mission.
Good post. I learn something new and challenging on sites I stumbleupon on a daily basis.
It’s always interesting to read content from other writers and use something from other web sites.
Just wanna comment that you have a very nice site, I love the layout it actually stands out.
Wow, awesome blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your site is excellent, as well as the content!
Having read this I believed it was extremely enlightening. I appreciate you
spending some time and energy to put this content together.
I once again find myself personally spending a significant amount of time both reading
and posting comments. But so what, it was still worth it!
I was suggested this website through my cousin. I am now
not positive whether this publish is written by way of him as no one else recognise such detailed about my trouble.
You are amazing! Thanks!
https://autolux-azerbaijan.com/# pin-up kazino
pin up giris: pin-up casino giris – pin up casino az
pin-up kazino https://azerbaijancuisine.com/# pin up onlayn kazino
pin up
Hey there! Someone in my Myspace group shared this website with us so I came to take a look. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Wonderful blog and amazing style and design.
Nearly all of what you mention is astonishingly appropriate and it makes me ponder why I had not looked at this with this light previously. This article truly did switch the light on for me personally as far as this topic goes. However there is actually one position I am not really too cozy with so while I attempt to reconcile that with the main theme of your position, let me observe what all the rest of your subscribers have to point out.Well done.
Everything is very open with a very clear clarification of the challenges.
It was definitely informative. Your website is very useful.
Thank you for sharing!
Great beat ! I would like to apprentice while you amend your web site, how could
i subscribe for a blog web site? The account helped me a
acceptable deal. I were tiny bit familiar of this your broadcast offered bright clear idea
Excellent article. I’m dealing with many of these issues as well..
Oh my goodness! Incredible article dude! Thank you so much, However I am experiencing issues with your RSS.
I don’t know why I can’t join it. Is there anybody getting identical RSS issues?
Anyone that knows the answer will you kindly respond?
Thanks!!
I always used to read post in news papers
but now as I am a user of internet therefore from now I am using net for articles, thanks to web.
Ahaa, its nice dialogue concerning this article here
at this website, I have read all that, so at this time me
also commenting here.
This text is priceless. How can I find out more?
Hi there i am kavin, its my first occasion to commenting anyplace,
when i read this article i thought i could also make comment due to this brilliant paragraph.
whoah this weblog is magnificent i love studying your articles.
Stay up the good work! You understand, many people are hunting around
for this information, you can help them greatly.
Excellent weblog right here! Additionally your web site a lot up very fast!
What host are you using? Can I get your associate link to your host?
I wish my web site loaded up as fast as yours lol
buying prescription drugs in mexico online: mexican pharmacy – buying from online mexican pharmacy
An impressive share! I’ve just forwarded this onto a colleague
who was doing a little homework on this. And he
actually ordered me lunch simply because I discovered it for him…
lol. So allow me to reword this…. Thanks for the
meal!! But yeah, thanks for spending some time to talk about this topic here on your
internet site.
Great web site you have here.. It’s difficult to find high-quality writing like yours nowadays.
I seriously appreciate people like you! Take care!!
medication from mexico pharmacy: mexican pharmacy online – mexico drug stores pharmacies
This info is invaluable. How can I find out more?
Heya i’m for the first time here. I found this board and I find
It really helpful & it helped me out much. I’m hoping to
provide one thing again and help others like you helped me.
mexican drugstore online northern doctors pharmacy mexico drug stores pharmacies
There is definately a lot to know about this subject.
I really like all the points you have made.
It’s fantastic that you are getting thoughts from this article as well as
from our dialogue made at this time.
I was recommended this website by my cousin. I’m not sure whether
this post is written by him as nobody else know such detailed about my trouble.
You’re wonderful! Thanks!
Hey I know this is off topic but I was wondering if you knew
of any widgets I could add to my blog that automatically tweet
my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have
some experience with something like this. Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new updates.
Article writing is also a excitement, if you
be familiar with afterward you can write or else it is difficult to
write.
Appreciating the commitment you put into your site and in depth information you present. It’s great to come across a blog every once in a while that isn’t the same out of date rehashed information. Fantastic read! I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
I’m impressed, I must say. Rarely do I encounter a blog that’s equally educative and interesting, and without a doubt, you have hit
the nail on the head. The issue is an issue that too few folks are
speaking intelligently about. I’m very happy I found this
during my hunt for something relating to this.
Some really superb articles on this internet site, thank you for contribution. “The difference between fiction and reality Fiction has to make sense.” by Tom Clancy.
Marvelous, what a blog it is! This blog gives valuable information to us, keep it up.
Howdy just wanted to give you a quick heads up.
The text in your content seem to be running off the screen in Firefox.
I’m not sure if this is a formatting issue or something to do with internet browser compatibility but I thought
I’d post to let you know. The style and design look great though!
Hope you get the problem solved soon. Cheers
Somebody essentially assist to make significantly posts I would state.
That is the very first time I frequented your website page and
thus far? I amazed with the analysis you made to make this actual submit extraordinary.
Excellent process!
This is a topic close to my heart cheers, where are your contact details though?
Wow! After all I got a webpage from where I can actually
obtain valuable information concerning my study
and knowledge.
I like the helpful info you provide in your articles.
I will bookmark your weblog and check again here frequently.
I am quite sure I’ll learn a lot of new stuff right here!
Good luck for the next!
hello there and thank you for your information – I have certainly
picked up anything new from right here. I did however expertise some technical points using this site,
as I experienced to reload the web site a lot of times previous to I could get it
to load properly. I had been wondering if your web host
is OK? Not that I am complaining, but sluggish loading instances times will sometimes affect your placement
in google and can damage your high-quality score if advertising and marketing with Adwords.
Anyway I’m adding this RSS to my e-mail and can look out
for much more of your respective interesting content.
Ensure that you update this again soon.
Great job site admin! You have made it look so easy talking about that topic, providing your readers some vital information. I would love to see more helpful articles like this, so please keep posting! I also have great posts about Data Mining, check out my weblog at http://counter.ogospel.com/cgi-bin/jump.cgi?http://webemail24.com/increase-your-online-income-through-email-marketing
This piece of writing will assist the internet users for setting
up new webpage or even a weblog from start to end.
Great post! I learned something new and interesting, which I also happen to cover on my blog. It would be great to get some feedback from those who share the same interest about Vintage/Antiques, here is my website http://chat.chat.ru/redirectwarn?http://seoranko.de/5-schritte-fuer-eine-gewinnbringende-website-seo-strategie Thank you!
Howdy! Quick question that’s entirely off topic. Do
you know how to make your site mobile friendly?
My website looks weird when viewing from my apple iphone.
I’m trying to find a theme or plugin that might be able to resolve this problem.
If you have any recommendations, please share. Thanks!
Fantastic goods from you, man. I’ve understand your stuff previous
to and you’re just extremely magnificent. I actually like what you’ve acquired here, really like what you are stating and
the way in which you say it. You make it entertaining
and you still take care of to keep it smart. I can’t wait to read much more from
you. This is actually a terrific web site.
Unquestionably imagine that which you stated. Your favorite justification seemed to
be at the internet the easiest factor to take note of.
I say to you, I certainly get annoyed while folks consider issues that they plainly do not recognise about.
You controlled to hit the nail upon the top as smartly as defined out
the entire thing without having side-effects , other people could take a
signal. Will probably be again to get more. Thanks
This info is priceless. How can I find out
more?
Hiya! Quick question that’s entirely off topic. Do you know how to
make your site mobile friendly? My site looks weird when browsing from
my iphone4. I’m trying to find a theme or plugin that might be able to correct this problem.
If you have any recommendations, please share. Appreciate it!
Thanks to my father who informed me on the topic of this blog, this webpage is
actually awesome.
Hi it’s me, I am also visiting this website on a regular basis, this site is really pleasant and
the people are in fact sharing nice thoughts.
Hi to every , because I am genuinely eager of reading this web site’s post to be
updated on a regular basis. It consists of good data.
I’m not that much of a internet reader to be honest but your sites really
nice, keep it up! I’ll go ahead and bookmark your site
to come back later on. Cheers
Nice blog here! Also your website quite a bit up fast! What host are you using? Can I get your affiliate hyperlink for your host? I wish my web site loaded up as fast as yours lol
Everything is very open with a very clear explanation of the challenges.
It was definitely informative. Your site is extremely helpful.
Thanks for sharing!
Hello! This is my first visit to your blog! We are a collection of volunteers and starting a new initiative in a community in the same niche. Your blog provided us useful information to work on. You have done a outstanding job!
I have to express some appreciation to the writer just for bailing me out of this particular circumstance. After looking out throughout the world wide web and coming across methods which were not beneficial, I figured my entire life was over. Being alive without the presence of solutions to the issues you have resolved as a result of your short post is a crucial case, as well as ones that might have negatively affected my entire career if I hadn’t come across the blog. That expertise and kindness in handling all things was invaluable. I am not sure what I would have done if I hadn’t encountered such a stuff like this. I’m able to at this moment look forward to my future. Thanks a lot very much for this specialized and result oriented guide. I won’t think twice to suggest your web site to anybody who will need recommendations about this issue.
Saved as a favorite, I really like your website!
Great post. I was checking continuously this blog and I am inspired!
Very helpful info specifically the closing phase 🙂 I deal with such info a lot.
I used to be seeking this particular info for a long time.
Thanks and good luck.
I love it when people come together and share opinions, great blog, keep it up.
Hi! I’ve been following your website for a long time
now and finally got the bravery to go ahead and give you a shout out from
Dallas Texas! Just wanted to mention keep up the excellent work!
Excellent post. I was checking continuously this blog and I’m impressed!
Very helpful info specially the last part 🙂
I care for such info much. I was looking for this particular information for a very
long time. Thank you and best of luck.
What’s Taking place i am new to this, I stumbled upon this I’ve found It absolutely useful and it has helped me out loads. I hope to give a contribution & help other users like its aided me. Great job.
This design is incredible! You definitely know how to keep a reader entertained.
Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Wonderful job.
I really loved what you had to say, and more than that, how you presented it.
Too cool!
I constantly emailed this blog post page to all my associates,
because if like to read it then my contacts will too.
An outstanding share! I’ve just forwarded this onto a friend who was conducting
a little research on this. And he in fact ordered me dinner due to the fact that I discovered it
for him… lol. So let me reword this…. Thanks for the
meal!! But yeah, thanx for spending some time to discuss this subject here
on your website.
Terrific article! That is the kind of info that should be shared around the net.
Disgrace on Google for no longer positioning this put up upper!
Come on over and consult with my site . Thank you =)
Heya just wanted to give you a brief heads up and let you know a few of the pictures aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different browsers and both show the same outcome.
Terrific article! That is the kind of information that are meant to be shared
around the web. Disgrace on the seek engines for not positioning this put up higher!
Come on over and visit my web site . Thanks =)
You really make it appear really easy along with your presentation but I find this topic to be actually one thing that I believe I
might never understand. It kind of feels too complex and very large for me.
I’m looking ahead on your subsequent put up, I’ll attempt to get
the hold of it!
I every time emailed this webpage post page to all my associates, because if like to read it afterward my contacts will too.
It’s appropriate time to make some plans for the future and it’s time to be happy.
I have read this post and if I could I want to suggest you some interesting
things or advice. Perhaps you could write next articles referring to
this article. I want to read even more things about it!
Thanks for sharing your thoughts on https://rglobalcarental.com. Regards
Can I simply say what a aid to seek out somebody who truly is aware of what theyre talking about on the internet. You undoubtedly know how to carry a difficulty to mild and make it important. More people have to learn this and perceive this aspect of the story. I cant consider youre no more widespread since you undoubtedly have the gift.
I visit each day some sites and sites to read articles
or reviews, except this blog gives quality based posts.
hello!,I like your writing so much! share we communicate more about your post on AOL? I require an expert on this area to solve my problem. May be that’s you! Looking forward to see you.
Hi, I think your website might be having browser compatibility issues. When I look at your website in Opera, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, superb blog!
Greetings from Los angeles! I’m bored to death at work so I decided to check out your website on my iphone during lunch break. I love the info you provide here and can’t wait to take a look when I get home. I’m surprised at how fast your blog loaded on my cell phone .. I’m not even using WIFI, just 3G .. Anyways, superb site!
mexican pharmaceuticals online: cmqpharma.com – mexican rx online
Some genuinely nice and utilitarian information on this site, likewise I conceive the style and design has got good features.
?»?best mexican online pharmacies
https://cmqpharma.online/# buying prescription drugs in mexico
buying prescription drugs in mexico
Usually I don’t learn post on blogs, however I wish to say that this write-up very forced me to try
and do it! Your writing taste has been amazed me. Thank you, very great article.
I have read so many posts on the topic of the blogger lovers
but this article is genuinely a pleasant
paragraph, keep it up.
Chic Hot Club: Womans Fashion Clothing Store At Chic Hot Club, We offer a curated selection of chic and trendy clothing pieces that inspire confidence and self-expression, at Competitive prices online.
It is not my first time to go to see this web site,
i am browsing this site dailly and obtain nice information from here daily.
Right now it looks like Expression Engine
is the best blogging platform available right now.
(from what I’ve read) Is that what you are
using on your blog?
There is noticeably a bundle to know about this. I assume you made certain nice points in features also.
At this moment I am going to do my breakfast, once having my breakfast coming yet again to read additional
news.
Explore Iceland in 3 days with a curated itinerary. Discover
Reykjavik’s charm, delve into wilderness adventures, savor Icelandic cuisine, and immerse in cultural treasures.
Learn weather conditions, driving laws, and full packing lists.
Book your Icelandic adventure now!
I am actually glad to read this weblog posts which carries plenty of useful data, thanks for
providing such data.
Very nice post. I simply stumbled upon your weblog and wished to say that I’ve really loved browsing your
blog posts. After all I’ll be subscribing on your rss
feed and I am hoping you write again soon!
Thanks for sharing your info. I truly appreciate your efforts and
I will be waiting for your next post thanks once again.
Have you ever considered writing an e-book or guest authoring on other sites?
I have a blog based on the same information you
discuss and would really like to have you share some stories/information. I know my audience would enjoy your work.
If you’re even remotely interested, feel free to shoot me an email.
You have observed very interesting details ! ps decent web site.
When some one searches for his required thing, thus he/she desires to be available that
in detail, so that thing is maintained over
here.
Today, I went to the beach front with my children. I found a sea shell and gave it to my 4
year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and
screamed. There was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is entirely off topic but I had to tell
someone!
What’s up colleagues, how is everything, and
what you wish for to say about this piece of writing, in my
view its genuinely amazing in favor of me.
You really make it appear really easy together with your presentation but
I find this matter to be actually something which I believe I would by no means understand.
It seems too complex and extremely wide for me.
I am looking ahead on your next put up, I will attempt to get the grasp of it!
These are actually impressive ideas in regarding blogging.
You have touched some good things here. Any way keep up wrinting.
Hello There. I found your blog using msn. This is a very well
written article. I will make sure to bookmark it and come back to read more of your useful info.
Thanks for the post. I will certainly comeback.
reputable indian online pharmacy: india pharmacy – reputable indian online pharmacy
http://foruspharma.com/# buying prescription drugs in mexico online
pharmacies in mexico that ship to usa: mexican border pharmacies shipping to usa – mexico drug stores pharmacies
https://doxycyclinedelivery.pro/# doxycycline 30
Wow, incredible weblog layout! How lengthy have you ever been running
a blog for? you make blogging look easy. The full
glance of your website is magnificent, as smartly as the content!
Please let me know if you’re looking for a author for your weblog. You have some really great articles and I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some content for your blog in exchange for a link back to mine. Please blast me an e-mail if interested. Thank you!
hello!,I love your writing so much! percentage we
communicate extra approximately your post
on AOL? I require a specialist on this house to solve
my problem. May be that’s you! Taking a look forward to
see you.
Feel free to surf to my site … ternate toto
Wow, awesome blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your website is magnificent,
let alone the content!
Excellent web site you have got here.. It’s hard to find high quality writing like yours nowadays.
I honestly appreciate people like you! Take care!!
Also visit my site; polototo
Someone essentially help to make seriously posts I would state.
This is the very first time I frequented your website page
and to this point? I amazed with the research you made to create this particular
put up extraordinary. Fantastic task!
Here is my site rajabandot
This blog was… how do you say it? Relevant!!
Finally I have found something that helped me. Thanks a lot!
my website miototo
I every time used to read post in news papers but
now as I am a user of web so from now I am using net for articles or reviews,
thanks to web.
Here is my page: polototo
I’m gone to tell my little brother, that he should also go to
see this webpage on regular basis to take updated from most up-to-date reports.
Hello Dear, are you in fact visiting this site daily, if
so after that you will definitely take nice knowledge.
The blog post provides a comprehensive 3-day travel itinerary for Utah, focusing on iconic natural landmarks and
adventurous activities. Plan your perfect 3-day trip to Utah
with visits to Arches National Park Bryce Canyon, Zion, Canyonlands, and adventures in Moab.