Geraldine Scott, Health Correspondent of the Eastern Daily Press, reports:
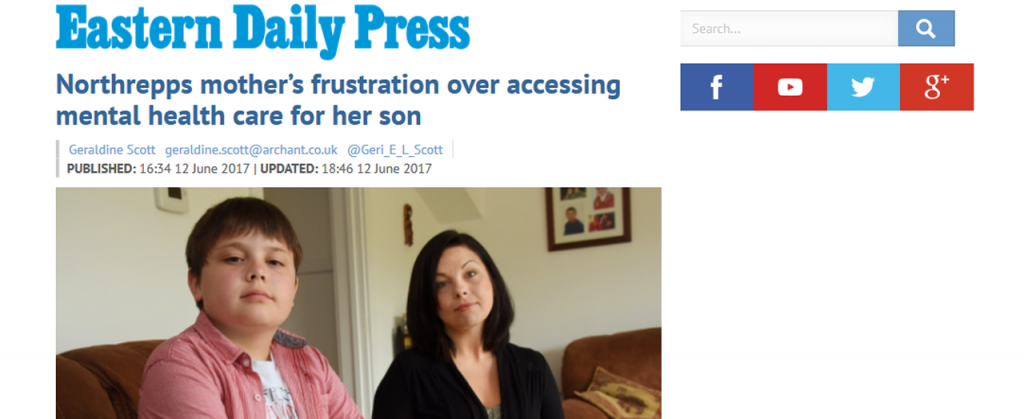
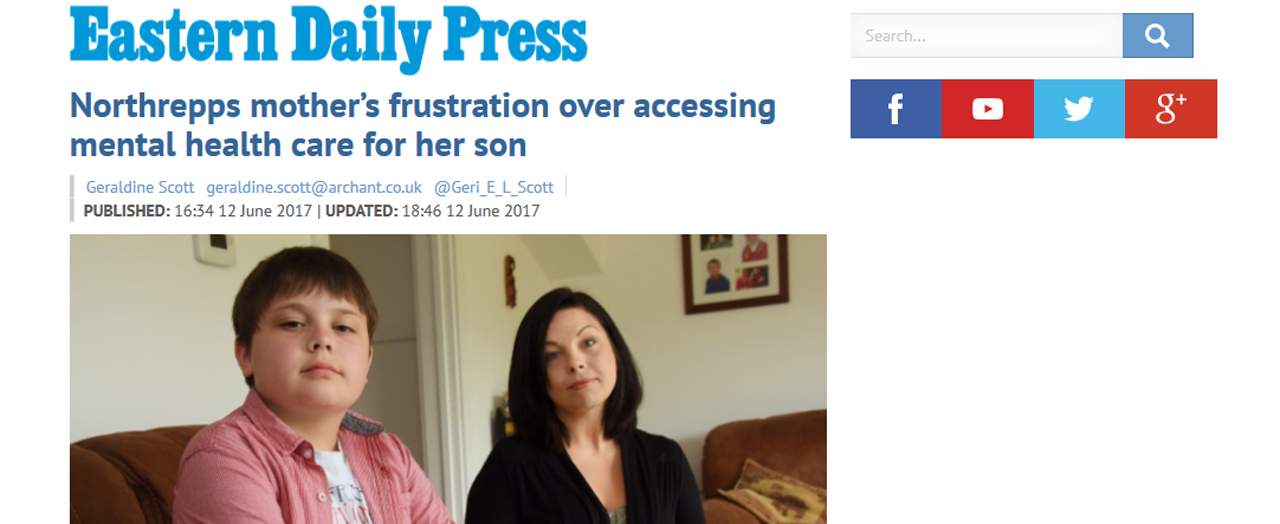
Michelle Kimp, 35, has struggled to get the appropriate medical treatment for her 12-year-old son Robert – who has aspergers and ADD – for around seven years.
Mrs Kimp said due to his conditions Robert had depression and had spoken about taking his own life.
But she said after bounced being between children and young people’s mental health services – known as CAHMS – and his paediatrician, she was told last November that “suicide is not necessarily mental health”.
“It was an incredibly long process to get a diagnosis in the first place,” said Mrs Kimp, who lives in Northrepps.
“The first time we went to CAHMS Robert had not been diagnosed at this point and they said he did not have a mental health problem.
“I said ‘he’s trying to kill himself, tell me that if I end up finding him dead’.”
Mrs Kimp is far from the first parent to be forced to say this to the Children, Family and Young Person (CFYP) Service.
Services for young people in Suffolk provided by Norfolk and Suffolk NHS Foundation Trust (NSFT) have already been condemned by a joint Ofsted/CQC inspection.
Mrs Kimp said she was particularly conscious of the risk as her cousin took his own life aged 16.
“It’s as if he’s got to seriously harm himself, harm someone else or kill himself before someone will help him,” she said.
No wonder the suicide rate in North Norfolk has increased by a staggering 77 per cent between 2010-12 and 2013-15.
Mrs Kimp believes the issues with treatment come because children on the autistic spectrum do not tick the right boxes.
“I went to a post diagnosis meeting a few weeks ago and was told this was normal because there isn’t the funding for autistic children with mental health. Because they present differently to ‘normal’ children with mental health issues, no one will treat them. It’s disgusting.”
Now, she wants to highlight how difficult the fight is, to try and raise awareness of the problem.
A spokesman for Norfolk and Suffolk NHS Foundation Trust, the region’s mental health trust, said young people with conditions such as Robert’s would usually be treated by their multi-disciplinary Neuro-Developmental Disorders Team and could stay with that team up to the age of 26.
They added: “We take suicidal thoughts or behaviours expressed by children and young people very seriously.
Why then has the suicide rate in North Norfolk increased by more than TWELVE times the national average increase?
“Every young person coming into our trust’s Children, Families and Young People’s services receive a full, and holistic assessment of their mental health needs, taking into consideration their social situation, family history and school or work life.”
This isn’t what we hear. Mrs Kimp’s experience is far from atypical.
CAMHS services at NSFT experienced the deepest cuts in England.
While patients waited months to be seen, one of NSFT’s CFYP consultants, on a salary of more than £150,000 per year, who was a coincidentally a trust cheerleader for the radical redesign cuts and establishment of ‘Youth’, was swimming and enjoying long lunches at UEA during the working day. We and others have raised the issue of ‘medical productivity’ at private meetings, at public NSFT Board meetings and personally with the Chair of NSFT, Gary Page, but no urgent or effective action is taken.
The Chair of NSFT and its executives know they have a minority of doctors on six-figure salaries who are seeing less than half a dozen patients in clinic per week but they are too weak or unbothered to do anything about a patently disgraceful situation. It is a Faustian Pact: the doctors don’t mention the appalling mismanagement, the management don’t address the minority of lazy doctors. But patients and their families pay the price.
To be clear, most doctors at NSFT work extremely hard. But a significant minority do not.
How can NSFT offer safe or effective secondary mental health services if some of its doctors aren’t seeing the patients in their area in clinic?
Patients, carers and front line clinical staff care deeply about waiting lists and lack of treatment but NSFT’s Board doesn’t seem to care about anything other than eating biscuits and drinking tea. There is no genuine voice of the patient and carer at NSFT.
NHS Improvement tried to help us bring about change on this vital issue but NSFT has even resisted its own regulator. We’ve been forced to go to local MPs – they find the situation outrageous. Physical health hospitals or GP practices wouldn’t tolerate doctors seeing one patient per day and nor should mental health.
New Ways of Shirking has to stop. If Bohdan Solomka is too weak to address this issue, NSFT needs a new external appointment to Medical Director.
Another consultant cheerleader for the disastrous radical redesign has a new job with the shiny-new perinatal service, now that Youth and EI services are under stress. When community mental health services were cut to shreds, the same cheerleader consultant left behind their slashed community mental health team and patients and took a new job with the shiny-new Youth Service. Despite £2.5m funding and an enormous salary bill for two consultants, the new perinatal service won’t start operating anything like fully until September. Time for more NSFT tea and biscuits. We hear from other areas of the country that their perinatal services have opened much more promptly. Don’t get ill if you’re pregnant, NSFT is in no rush.
Even more worryingly, we hear that NSFT has adopted its own definition of perinatal mental health which means that women with existing mental health conditions won’t be able to access the full service – just those who are ‘pure’ and have developed mental health problems for the first time during pregnancy. Women with existing mental health conditions who become pregnant have to stay in the generic and overwhelmed community mental health teams, apparently.
If true, we’d say that’s shocking discrimination.
Click on the image below to read the story in full on the EDP website:
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
???? ???? Often. In most cases, fraudulent companies buy legitimate dolls and then recreate a much cheaper version, stealing the original photo from another website and using it to fool unsuspe
pin-up https://azerbaijancuisine.com/# pin up 360
pin-up
pin up azerbaijan: pin up azerbaycan yukle – pin-up kazino
medicine in mexico pharmacies: mexican pharmacy online – best online pharmacies in mexico
http://northern-doctors.org/# mexican pharmacy
?»?best mexican online pharmacies: mexican pharmacy – mexican border pharmacies shipping to usa
https://northern-doctors.org/# mexican drugstore online
mexico pharmacy: northern doctors – purple pharmacy mexico price list
pharmacies in mexico that ship to usa mexican pharmacy mexican online pharmacies prescription drugs
https://northern-doctors.org/# medicine in mexico pharmacies
buying prescription drugs in mexico: Mexico pharmacy that ship to usa – pharmacies in mexico that ship to usa
https://northern-doctors.org/# mexican rx online
mexican pharmaceuticals online: mexican mail order pharmacies – mexico pharmacy
mexican mail order pharmacies mexican pharmacy online reputable mexican pharmacies online
purple pharmacy mexico price list: mexican pharmacy northern doctors – medication from mexico pharmacy
mexican drugstore online: mexican northern doctors – purple pharmacy mexico price list
mexican online pharmacies prescription drugs: mexican pharmacy – reputable mexican pharmacies online
mexican pharmacy: mexican pharmacy online – mexican drugstore online
reputable mexican pharmacies online: northern doctors pharmacy – mexico pharmacies prescription drugs
https://northern-doctors.org/# mexican pharmaceuticals online
mexican pharmacy: mexican pharmacy online – mexico drug stores pharmacies
reputable mexican pharmacies online: mexican pharmacy online – mexican rx online
http://northern-doctors.org/# mexico drug stores pharmacies
mexican pharmaceuticals online: mexican pharmacy – mexican online pharmacies prescription drugs
mexico drug stores pharmacies northern doctors pharmacy medicine in mexico pharmacies
https://northern-doctors.org/# mexican rx online
mexico drug stores pharmacies: mexican pharmacy – mexico pharmacy
https://northern-doctors.org/# buying prescription drugs in mexico
mexican mail order pharmacies: medication from mexico pharmacy – ?»?best mexican online pharmacies
mexican online pharmacies prescription drugs: northern doctors pharmacy – buying prescription drugs in mexico
mexican online pharmacies prescription drugs: mexican pharmacy – mexico drug stores pharmacies
https://northern-doctors.org/# mexican rx online
mexico drug stores pharmacies: mexican pharmacy – mexican online pharmacies prescription drugs
mexican pharmacy: mexican pharmacy northern doctors – pharmacies in mexico that ship to usa
mexico drug stores pharmacies: northern doctors pharmacy – reputable mexican pharmacies online
reputable mexican pharmacies online: mexican pharmacy northern doctors – mexico pharmacy
mexico drug stores pharmacies northern doctors pharmacy mexico drug stores pharmacies
https://northern-doctors.org/# mexico pharmacy
medication from mexico pharmacy: mexican pharmacy northern doctors – mexican rx online
best online pharmacies in mexico: northern doctors – medication from mexico pharmacy
?»?best mexican online pharmacies: Mexico pharmacy that ship to usa – mexico drug stores pharmacies
mexican border pharmacies shipping to usa: mexican pharmacy – mexico pharmacy
buying from online mexican pharmacy mexican pharmacy purple pharmacy mexico price list
mexican rx online: mexican pharmacy northern doctors – mexico pharmacy
https://northern-doctors.org/# mexican online pharmacies prescription drugs
medication from mexico pharmacy: Mexico pharmacy that ship to usa – buying from online mexican pharmacy
buying from online mexican pharmacy: medicine in mexico pharmacies – medicine in mexico pharmacies
mexico pharmacies prescription drugs: mexican pharmacy – medicine in mexico pharmacies
http://cmqpharma.com/# mexican pharmacy
buying prescription drugs in mexico online
mexico pharmacy mexican online pharmacy mexican pharmacy
mexico pharmacy: reputable mexican pharmacies online – buying prescription drugs in mexico online
mexican mail order pharmacies mexico pharmacy mexico pharmacy
medicine in mexico pharmacies
https://cmqpharma.com/# pharmacies in mexico that ship to usa
purple pharmacy mexico price list
mexican mail order pharmacies mexican pharmacy reputable mexican pharmacies online
mexico drug stores pharmacies mexico pharmacy mexican mail order pharmacies
mexican online pharmacies prescription drugs cmqpharma.com mexico pharmacies prescription drugs
mexico pharmacies prescription drugs: mexico drug stores pharmacies – mexican drugstore online
mexican border pharmacies shipping to usa: mexican online pharmacies prescription drugs – mexican drugstore online
http://foruspharma.com/# buying from online mexican pharmacy
reputable mexican pharmacies online buying prescription drugs in mexico mexico pharmacy
indian pharmacies safe: cheapest online pharmacy india – indian pharmacies safe
canadian pharmacy meds: canadian pharmacy meds – canada drugs online
indian pharmacies safe: online pharmacy india – mail order pharmacy india
ordering drugs from canada canadian valley pharmacy canada pharmacy 24h
http://indiapharmast.com/# indian pharmacy
buying from online mexican pharmacy: mexican pharmaceuticals online – mexican pharmaceuticals online
indianpharmacy com: india pharmacy – indian pharmacy paypal
online canadian pharmacy review: canadian discount pharmacy – canadian pharmacy meds
https://canadapharmast.com/# canadian pharmacy reviews
canadapharmacyonline: global pharmacy canada – reputable canadian pharmacy
online canadian pharmacy reviews: safe canadian pharmacy – canadian pharmacy meds
https://amoxildelivery.pro/# buy amoxicillin online mexico
https://amoxildelivery.pro/# how to buy amoxicillin online
https://ciprodelivery.pro/# buy cipro online without prescription
https://clomiddelivery.pro/# can i get generic clomid without rx
http://clomiddelivery.pro/# cost of clomid now
http://ciprodelivery.pro/# ciprofloxacin
http://amoxildelivery.pro/# amoxicillin script
http://amoxildelivery.pro/# medicine amoxicillin 500
https://clomiddelivery.pro/# can you get cheap clomid price