We haven’t been able to publish the devastating review into the shocking death of Neil Jewell as a jury inquest has been taking place.
However, we can now publish the Safeguarding Adult Review (SAR) into Neil’s death in full.
We’d like to express our admiration for Neil Jewell’s family for their determination: they have lived in a camper van for the three weeks of the inquest and have been battling for justice for more than three years since he died at the age of just 42. As the review makes clear, Neil’s family fought for many years for Neil’s welfare, tirelessly but sadly in vain, before he died. They and Neil deserve better than ‘it was a long time ago’, ‘we’re on a journey’ or ‘lessons will be learned’.
Mr. Jewell died, miles away from home, just two months after our campaign was founded to warn of exactly the dangers which cost Neil Jewell his life. Despite being aware of the circumstances of Neil’s death, with one its most senior managers being a member of the review, the mental health trust which let Neil down, Norfolk and Suffolk NHS Foundation Trust (NSFT), continued wasting millions of pounds making health professionals redundant as it cut mental health beds and services. In fact, mental health services in Norfolk deteriorated further when social workers from Norfolk County Council and NHS staff from NSFT were forced to stop working together in the same teams when the Section 75 Agreement between them broke down in acrimony.
If Neil had continued to receive the high quality community support and prompt admission to a proper local NHS hospital at times of crisis, he would probably still be alive. NHS and social services reviews need to start telling the truth about inadequate resources rather than talking about ‘communications’ and blaming individual staff rather than funding cuts. Nothing discriminates more against people with mental health needs than the denial of prompt and professional help.
Gary Page, the Chair of NSFT, ignored our warnings and dismissed the catastrophic collapse of mental health services as a ‘so-called crisis’ as he insisted that job cuts and bed closures had to continue.
Commissioners at the clinical commissioning groups (CCGs) failed to fund mental health services properly yet found the cash to give themselves substantial pay rises.
In the same month that Neil Jewell died, commissioners and NSFT promised that there would be no more out of area placements after the end of April 2014. Yet the beds crisis has become worse and worse as commissioners and NSFT have broken their promises and blown their budgets month after month after month.
Just as happened at Mundesley Hospital, NSFT’s Board showed little apparent interest in the quality of the premises to which it sent Neil Jewell: all that mattered was that service users were off the books, so the executive tea drinking and biscuit dunking could resume: as Neil’s support worker and other mental health staff were made redundant and beds were closed, the number of NSFT managers increased.
Neil Jewell was sent to Hamilton House for Clozapine re-titration when NSFT didn’t have enough beds. Again, as at Mundesley Hospital and NSFT itself, it took the CQC to uncover inadequate standards of care.
The Minister of State at the Department of Health responsible for mental health while Neil Jewell died was local MP and self-proclaimed ‘mental health champion’, Norman Lamb. Reading the report, it appears that as his health deteriorated, Neil had more contact with employment advisers and benefits assessors than he did with the NHS and that the stress of these encounters made his health worse. What a fine job Norman Lamb did!
NSFT’s Board claimed it didn’t have enough money for decent health services but has found more than half a million pounds for Chief Executive Michael Scott’s salary over the last three years since the unnecessary death of Neil Jewell.
At NSFT’s most recent Board meeting, we read out the summary from the report below, referring to Neil as AA so as not to influence the inquest underway. As we did so, the Chief Executive, Michael Scott, drummed his fingers impatiently on the table in front of him and chatted to the Chair, Gary Page. We even had to ask Michael Scott to be quiet and listen to the circumstances of Neil’s death. Should we have to ask that of the Chief Executive of an NHS trust? Why did none of the other members of the Board of Shame take issue with Michael Scott’s behaviour which we are pursuing with local MPs and the regulator of NHS trusts, NHS Improvement? How can ‘lessons be learned’ when the Chief Executive isn’t listening?
The NSFT Chief Executive, Michael Scott, didn’t express any sorrow over what happened. He didn’t even respond until prompted to do so by the Chair, Gary Page. All Michael Scott would say was that he was pleased with the ‘improvements’ made. We don’t understand how it is an improvement for the number of NSFT patients who have died to double or for the beds crisis to become much worse. NSFT responded to the increasing number of deaths by removing all record of them from its own Annual Report.
The review doesn’t say so directly but we know that the reason so many patients were discharged from Care Programme Approach (CPA) was because NSFT didn’t have enough staff to implement it. Link workers, who worked with GPs to keep people like Neil well, were abolished. The Assertive Outreach teams that engaged with people like Neil were closed. The mental health base in the city of Norwich where Neil lived was closed: many mental health staff were moved to a business park outside Wymondham which still lacks facilities to see patients.
When doctors objected to the cuts, they were called ‘shroud wavers’. Trade unionists were victimised, false and irrelevant accusations about sex lives discussed by NSFT executives who should have been working to improve mental health services rather than demanding that campaigning staff were ‘got rid of’. Service users and carers have been ignored or marginalised with genuine co-production virtually non-existent. When we hold the NSFT Board to account and raise the cuts, job losses, complacency, broken promises, incompetence, wasted millions, denials, pay rises and deaths, NSFT directors accuse us of ‘personal attacks’ and spend thousands of pounds of NHS funds on lawyers.
Neil’s death is one of far too many.
Enough is enough.
The Crown Prosecution Service (CPS) may have decided that there was insufficient evidence to prosecute NSFT but NSFT’s Board should at least face the court of public opinion. If the inquest has produced new evidence, NSFT should be prosecuted.
Don’t forget that when we raised the issue of the increasing number of deaths at the NSFT Board meeting in Swaffham, shortly after Neil Jewell’s death, an NSFT Director demanded that our questions were struck from the minutes. Disgracefully, he still sits on NSFT’s Board of Shame.
It wasn’t a ‘so-called crisis’, Mr Page. It was and is a crisis.
While Gary ‘investment banker’ Page lives in luxury post banking crisis, mental health patients die of neglect and in squalor as a result of the cuts Gary Page and his Board insisted were necessary and safe. Why should those in greatest need pay the price of the bankers’ greed?
Only an ‘investment banker’ would cling onto his job at the top of an organisation in circumstances such as these. Sadly, the NSFT Chair, Gary Page, is an ‘investment banker’: Gary Page showed his true colours when he closed the last NSFT Board meeting half an hour early rather than answer questions from the public.
We will have a lot more to say about the cuts and chaos that led to Neil Jewell’s death over the coming weeks. We find the details of workplace bullying of Neil Jewell very distressing. We should have no place in our society for stigma.
Join us on the March for Mental Health on Sunday 30th April at 11 a.m. on Norwich City Hall steps.
The shocking Safeguarding Adult Review in respect of Mr Neil Jewell is published below.
We have replaced the use of AA with Neil’s real name and highlighted some key passages. The people who have died as a result of the cuts and incompetence at NSFT are not initials or statistics.
Norfolk Safeguarding Adults Board and Suffolk Safeguarding Adults Board
Safeguarding Adult Review in respect of Mr Neil Jewell
Died January 2014
Deborah Klée
Overview Report Writer
June 2015
Acknowledgements:
A number of people have given valuable support in the preparation of this report. In particular thanks are extended to: Tim Beach, Jane Brammer, Saranna Burgess, Jan Cant, Simon Chase, Jo Cook, Dr. Alison Dow, Roy Elmer, Tracey Fordham, Mike Garwood, Jim Gooding, Joan Maughan, Roger Morgan, Andy Ninham Shona Noon, Julie Sadler, DCI Andy Smith, Howard Stanley, Helen Thacker, Colin Van-Lint, Julie Wvendth, Paula Youell,
Perhaps most significant was the contribution offered by Neil Jewell’s family. The insight they provided has served to greatly enrich the depth and quality of the review. In doing so, they have supported the learning and development by agencies working with other adults at risk in Suffolk and Norfolk.
Summary
Neil Jewell was a quiet and gentle man who lived with paranoid schizophrenia. In the early years following diagnosis Neil received CPA (Care programme approach) and was supported by a care coordinator that he knew and trusted. Despite Neil’s self neglect and poor motivation his care coordinator and other community support workers gained his trust and were able to enrich his life with opportunities to socialize. When Neil experienced mental health crisis he received timely and appropriate support. He knew who to contact and what to expect.
This all changed in 2011 as a result of organisational change in the mental health trust. A cost improvement strategy meant that Neil’s care coordinator was made redundant and the level of care and support that Neil received reduced dramatically. Neil was discharged from CPA in July 2013. This started a series of events that tragically led to Neil’s death in January 2014.
When Neil presented himself at the Clozapine Clinic in January 2014 to report that he had run out of Clozapine medication four days ago and was feeling unwell, it was because he would not have known whom else to contact.
A decision was made to admit Neil to a local care home for re-titration on Clozapine. This means gradually building up his tolerance, as suddenly stopping or starting this medication can have a negative impact on physical and mental health. The only suitable hospital bed was in London, so the local care home was considered a better option.
A risk assessment was carried out but it was based on Neil’s last CPA review and that was ill informed, as the care coordinator did not know Neil well. Neil was admitted to the care home with a risk assessment and care plan that did not address how challenging behaviours would be managed, what the roles were of different agencies and professionals and how concerns might be escalated.
Neil became very agitated in the care home. As Neil’s behaviour became more challenging the care home sought help from the Crisis and Resolution Home Treatment team, an approved mental health practitioner (to carry out a mental health act assessment for section 2 and arrange admission to hospital) and the police, to help manage Neil. The roles of professionals in different agencies were not clear. The police were asked to intervene in a situation that required the expertise of a mental health professional.
Neil was handcuffed and strapped prone to a stretcher using external restraint belts to transport him to hospital in the neighbouring county of Suffolk. There were no beds in Neil’s home county of Norfolk. Neil was eventually admitted to a psychiatric intensive care unit bed. Staff at the hospital had little information about Neil. They saw a man who was handcuffed and strapped down and responded by treating him with caution. Neil was secluded (supervised confinement) as a result.
Neil was observed whilst in seclusion and when a member of staff noted that he had not moved for sometime he was found to have stopped breathing. Neil was resuscitated and admitted to Ipswich General Hospital where he died five days later when his life support machine was turned off.
A number of events led to Neil’s tragic death in January 2014.
This started with the care and support that Neil needed to live independently in the community being withdrawn due to a reduction in staff.
Neil was discharged from CPA despite meeting the criteria, because the care coordinator and medic making the decision did not know Neil and did not involve his family.
When Neil ran out of medication and became unwell he did not have a health and social care support network to help him manage the crisis. A risk assessment and plan was prepared but was not based on a knowledge and understanding of Neil.
The lack of an informed risk assessment and comprehensive plan meant that there was no plan for managing Neil’s challenging behavior and de-escalating it. As a result poor decisions were made regarding control and restraint and there was confusion over the roles and responsibilities of the professionals involved.
Neil was restrained with handcuffs and straps lying prone on a stretcher. This gave a false impression to staff in the admitting hospital that he was a danger to others. Neil was secluded and proper health checks were not carried out.
Neil’s health would have been at risk due to the combination of drugs – sedatives and clozapine, being positioned in the prone position for nearly two hours, repeated head banging, dehydration through a lack of fluids and sudden withdrawal from Clozapine.
There was no one incident that led to Neil’s death. The SAR report shows how one incident impacted on another so that staff found themselves in circumstances where they did not have the information, knowledge or resources to make good decisions.
The report makes recommendations for partners to work together to:
- effectively support people who self neglect;
- involve the person and their family as appropriate in planning care;
- consider the impact of organisational change on adults at risk;
- improve the quality of multi agency risk assessment and joint decision making when managing complex cases;
- improve information sharing;
- ensure the appropriate use of all types control and restraint methods
1.0 Background
1.1 Neil Jewell, a 42 year old man living with paranoid schizophrenia, died in January 2014 in Ipswich Hospital. The Home Office Approved Pathologist gave the cause of death as brain damage as a result of cardiac arrest and pneumonia.
1.2 Neil was diagnosed with paranoid schizophrenia in 2005. Following a period of hospitalization and rehabilitation at a supported living unit Neil was discharged to live independently in a council flat. He had a Care Programme Approach (CPA) plan and this was implemented with care coordinator support.
1.3 Between 2007 and 2011 Neil was supported by care coordinators that knew him well. When there were crisis the community team responded quickly and appropriately. In 2011 this changed and the level of community support provided to Neil was greatly reduced. He was discharged from CPA in July 2013.
1.4 In January 2014 Neil presented himself at the Clozapine Clinic to tell them that he had run out of medication over the Christmas holiday period and so had not taken his medication for four days. The following day Neil was admitted to a care home as a voluntary patient to build up his tolerance to Clozapine whilst under observation.
1.5 During his stay at the care home Neil’s condition deteriorated and his disturbed, agitated behavior became a risk for himself and those around him. He was sectioned under the Mental Health Act Section 2 and arrangements were made to admit him to Wedgewood House (West Suffolk) as there were no beds available in Norfolk (his place of residence).
1.6 Neil was transported by ambulance escorted by two police officers. He was handcuffed and restrained with straps to a stretcher on which he was lying prone.
1.7 Although an open ward had originally been planned for Neil this was changed to a psychiatric intensive care unit (PICU) bed when his condition deteriorated. A PICU bed was not immediately available and so Neil was held first on a 136 suite and then in seclusion (a locked bedroom, with observation checks every 15 minutes).
1.8 Neil was transferred in a secure private ambulance to Ipswich PICU later that evening. Neil was observed throughout the day but concern was raised when he was found to have stopped moving. Cardio pulmonary resuscitation (CPR) was carried out and emergency services called.
1.9 Neil was transferred to Ipswich General Hospital where he died, five days later, on the 17th January when his life support machine was turned off.
2.0 Purpose and Terms of Reference
2.1 The purpose of a Safeguarding Adults Review (SAR) is neither to investigate nor to apportion blame. It is only relevant when professionals can learn lessons and adjust practice in the light of lessons learnt. It therefore requires outcomes that:
- Establish what lessons can be learnt from the particular circumstances of a case in which professionals and agencies work together to safeguard adults
- Identify what those lessons are, how they should be acted upon and what is expected to change as a result.
- Review the effectiveness of procedures, both of individual organisations and multi-agency arrangements
- Improve practice by acting on the findings (developing best practice across organisations)
- Improve inter-agency working to better safeguard adults
- Make a difference for adults at risk of abuse and neglect.
2.2 The Terms of Reference of this Safeguarding Adult Review are:
- To examine the care and treatment Neil was receiving at the time of the incident, to ensure correct processes, protocols and procedures were followed and required standards were met.
- To consider whether Neil’s physical health needs were given due care and attention
- To respond to questions raised by family members, with particular reference to the communication between the Crisis Team and Hamilton House.
- To explore the effectiveness of communications policies and systems between identified providers of services.
- To determine the levels of authority in decision making when transporting patients with a significant psychiatric illness. Detailing ultimate responsibility between Police; Approved Mental Health Practitioner and Ambulance Trust staff.
- To examine if existing Policies align in respect of the transporting of patients.
- To consider the appropriateness of significant restraint and the requirement to monitor and review its application.
- To explore the practices in recording medication when prescribed/issued are adequate.
- To consider if any resource/acute bed availability had an impact
- To consider if the monitoring of Neil was at a sufficient level in regard to his medication regime and the ability to position him to limit the risk of asphyxiation in both his transport arrangements and care in seclusion area.
- To gain an understanding of the ability of staff to respond to an emergency in seclusion areas.
- To consider if the monitoring of Neil was at a sufficient level in the community in regard to his care, including his medication regime and his ability to maintain an appropriate living environment.
- To consider if the recommendations of a previous inquiry HSG(94)27 in regard to Mr David Bennett were not complied with by all agencies.
- To make recommendations for improvements, which agencies can use to inform existing policies and practice.
- The Safeguarding Adults Boards should aim for completion of a Safeguarding Adults Review within a reasonable period of time and in any event within six months of initiating it, unless there are good reasons for a longer period being required; for example, because of potential prejudice to related court proceedings. Every effort should be made while the Safeguarding Adults Review is in progress to capture points from the case about improvements needed; and to take corrective action.
- Review to cover the three month period prior to the death of Mr Neil Jewell. Any influencing organisational factors outside this timeframe to be referenced by the Independent Management Review writers.
2.3 The emphasis in this review is on the lessons and implications for multiagency working. Individual Management Reports (IMRs) have been prepared by all agencies involved with Neil Jewell and deal in detail with the actions required within each individual agency. The Safeguarding Adults Partnership Boards will provide a scrutiny role in relation to single agency action plans but those individual actions/recommendations will only be included in the SAR overview report recommendations where:
- they have significant implications across agencies.
- they underline highly pertinent matters which may have received tepid attention in the IMR recommendations – and the Safeguarding Adults Board needs to be alert to them.
3.0 The Review Process
3.1 A criminal investigation was undertaken by the Suffolk Constabulary Joint Major Investigation Team on the unexplained death of Neil Jewell, Operation Madeley. On the 11th January 2015 Norfolk and Suffolk safeguarding Adult Boards received confirmation that the Crown Prosecution Service advised that there was insufficient evidence to warrant criminal prosecutions of either individuals or organisations involved in the care of Neil Jewell [1].
3.2 Statutory guidance for the Care Act 2014, states that ‘a criminal investigation by the police takes priority over all other enquiries.[2] It also recommends that ‘early contact with police may assist in obtaining and securing evidence and witness statements’.[3]
3.3 The Joint Major Investigations Team, made a safeguarding referral to Suffolk Social Care in January 2014. The safeguarding adult investigating officer’s report [4] recommended that an adult safeguarding strategy meeting be convened on the conclusion of the police investigation ‘to consider whether there is learning to be shared with other agencies.’
3.4 A safeguarding adult review (SAR) advisory panel was convened on the 6th October 2014 with representatives from the Norfolk and Suffolk safeguarding adults boards. It was agreed at this meeting that the Neil Jewell case met the full criteria for a safeguarding adult review (SAR) and a recommendation was made to the two boards to this effect. The draft terms of reference for the SAR were agreed at a SAR advisory panel meeting on the 12th November.
3.5 The SAR panel included:
- Jo Cook Operational Head of Integrated Care- Northern Locality – Adult Social Services (Chair of the SAR panel)
- Joan Maughan – Independent Chair Norfolk Safeguarding Adults Board
- Tim Beach Independent Chair Suffolk Safeguarding Adults Board
- Helen Thacker – Safeguarding Adults Board Manager, Norfolk
- Roy Elmer – Safeguarding Adults Board Manager, Suffolk
- Saranna Burgess – Assistant Director of Nursing Norfolk and Suffolk NHS Foundation Trust
- Mike Garwood Solicitor
- Roger Morgan – Quality Assurance Manager, Adult Social Services
- Shona Noon – Prime Life
- Julie Wvendth – Norfolk Police
- Andy Smith – Suffolk Police
- Howard Stanley Norfolk CCGs
- Paula Youell – Suffolk County Council
- Jan Cant – Business Support Officer, Norfolk Safeguarding Adults Board.
[1] Email from DCI Andy Smith 11/01/2015 (D176)
[2] Care and Support Statutory Guidance issued under the Care Act 2014, June 2014 Department of Health, London pp.249 (14.75)
[3] pp. 192 (14.71)
[4] Suffolk Adult Safeguarding Board, Investigating Officer’s Report (IOR1), 24th June 2014 Suzanne Ludlow
3.6 Organisations that had significant involvement with Neil in the three months prior to his death, completed a chronology of events outlining their involvement. These were collated into an integrated chronology. The integrated chronology starts in 2005 when Neil was diagnosed with paranoid schizophrenia and finishes in January 2014. The extended chronology was requested by the overview report writer in response to concerns raised by Mr Neil Jewell’s sister regarding the care and support received by Neil prior to December 2013.
3.7 Internal management reviews (IMRs) were requested from all of the organisations that had significant involvement with Neil. A chronology and IMR was requested and received from the following organisations:
- East Anglian Ambulance Trust
- Ipswich Hospital NHS Trust
- Norfolk Constabulary
- Norfolk County Council, Adult Social Services
- Norfolk and Suffolk NHS Foundation Trust
- Norwich City Council, Housing
- Prime Life
- Prospect Medical Practice
- Suffolk Constabulary
- UK Special Ambulance Service (UK SAS)
- Department of Work and Pensions
3.8 The Joint Major Investigation Team, Suffolk Police made available all documents relating to Operational Madeley, on request. These included witness statements, CCTV images and expert opinions. Documents shared with the overview report writer are listed in appendix one.
3.9 Neil’s sister and brother-in-law were interviewed by the serious case review overview report writer at the outset of the review to get their views and perspective on Mr Neil Jewell’s experience of care and support. Questions raised by Neil’s sister and brother-in-law informed the terms of reference of the SAR.
3.10 The SAR panel met in April 2015 to consider the IMR reports. The IMR writers made presentations to the SAR panel, answered questions and contributed to discussions. The purpose of this meeting was for the panel to start to identify some of the lessons learnt.
4.0 A Pen Picture of Neil Jewell
Unless otherwise stated, the following information is based on a witness statement by Neil’s sister [5] and the transcription of the overview report writer’s interview with Neil’s sister and brother-in-law on the 30th January 2015. Comments in italics are the author’s observations.
4.1 Neil was 42 years old when he tragically died. He was born in Surrey, the youngest of three children. He had an older brother and sister. His brother was 13 years old and his sister 12 years old at the time of his birth. It was an unexpected pregnancy for his mother who was aged forty at the time.
4.2 Neil did not have much contact with other children prior to starting infant school. He went to a playgroup for a very short time but when he bit a child his mother decided to withdraw him from the playgroup. His sister remembers that he was a happy, smiling toddler, full of fun following super heroes and the usual boy games and toys.
4.3 When Neil was six years old his parents started divorce proceedings. His mother had difficulty managing her affairs and depended upon her 17 year old daughter (Neil’s sister) for assistance. Following the divorce Neil’s older brother stayed in the family home with his father and Neil, his sister and mother moved to a maisonette in Surrey. Neil visited his father and brother every other weekend for a few months and then all contact ceased.
4.4 As Neil grew up he had very few friends. School reports, as early as primary school, say that he was lacking in confidence, easily led by his peers and struggling to concentrate. In secondary school he enjoyed woodwork and other ‘hands on’ subjects but never took the CSE in maths and struggled in other subjects. He was bullied at school. Students would take his lunch away from him and as a result he didn’t take in any lunch and went hungry. Neil seemed to accept this and never complained.
4.5 Neil’s sister helped him to enroll at Norwich City College when he left school. The plan was for Neil and his mother to move to Norfolk to be closer to Neil’s sister. However, it took some time to sell his mother’s maisonette and for her to buy a house in Norfolk and so for ten months Neil lived with his sister and brother-in-law. Neil left Norwich City College with a City and Guilds fabrication, welding and plumbing certificate.
4.6 As an adult Neil’s sister describes his mental capacity and ability as that of a young teenager. ‘Neil couldn’t make decisions, he lacked the ability to engage in conversation with people and he had no real social skills. He found moving into the adult world a huge challenge. Tasks, which others would have undertaken with ease, would have caused Neil anxiety and stress. He had never had a group of friends, a girlfriend or anyone close to him other than his mother. He was capable of riding a moped, driving a car and doing jobs but he would have stood out as different to his peers and was vulnerable to being taken for granted, used and manipulated.’
[5] Witness statement Neil’s sister – Operation Madeley
4.7 Between 1989 and 2002 Neil had a number of jobs including, plumbing, retail, and Anglian Water. However, there was a history of bullying by colleagues, for example filling his boots with glue and sending him on errands as ‘pranks’. One colleague would get Neil to pay for his lunch every day. During this period when Neil was unemployed for a period between jobs he became depressed. He enjoyed work but understandably, given his lack of social skills and experience of bullying, found it difficult working with others.
4.8 Neil’s mental health deteriorated when he left his last job in 2002. By 2005 he had become physically violent towards his mother. He started hearing voices and hallucinating. In 2005 Neil’s behaviour became too much for his mother and so she went to the GP for advice. When his mother had been gone for some time Neil went to the GP surgery to find her. The GP took this opportunity to make arrangements to admit Neil to an acute ward under section 2 of the Mental Health Act. Following admission Neil climbed out of the window at night and walked back home. This was a journey of around 10 miles. He was then sectioned and readmitted again under section 2.
4.9 When Neil was ready to be discharged there wasn’t a council property available and so he was discharged to bed and breakfast accommodation whilst permanent accommodation was being sought. One week after being sent to the bed and breakfast accommodation Neil took an overdose and asked the owner of the bed and breakfast to call an ambulance for him. Neil was readmitted to Hellesdon Hospital. His sister said that Neil had been getting pre-packed sandwiches from the nearby garage. He had been given a map to the nearest supermarket but his sister said, ‘It was a very long walk for Neil even if he had chosen to go there. He wouldn’t have been able to consider getting the bus as he wouldn’t have had the necessary thought processes to do so. Also Neil couldn’t have read the map so this was completely useless to him.’
4.10 Neil’s sister was not informed by the hospital that Neil had been discharged. Neither was she told that he had taken an over dose and been admitted to hospital. It was only when the family could not contact Neil that they phoned around and found out he had taken an overdose and been admitted to hospital.
4.11 In 2006 Neil was placed in Oak Hose, a Julian Housing facility. Here he received rehabilitation to help him develop skills such as cooking and self care.
4.12 In 2007 Neil moved into a flat. He seemed pleased and happy with the flat but soon after settling there he took an overdose. He became paranoid focusing on the behaviour of his neighbours.
4.13 Between 2007 and 2012 Neil was supported to live independently in the community. He had regular contact with a support worker, first a woman and then a man. He had a good relationship with both of them. During this period he enjoyed a couple of camping trips, learnt how to use a laptop computer and enjoyed activities and outings with a small group of other young men. Neil attended a weekly coffee club and enjoyed cycling. He had a weekly timetable and was prompted to follow it by his community support worker. His community support worker was planning to take a group of men including Neil on a holiday to Turkey, when his post was made redundant. Neil had even got himself a passport. Neil’s sister said ‘Neil’s life was enriched when he had support from a community support worker that he trusted.’ This was a relatively good period in Neil’s life.
4.14 Between 2012 and 2014 Neil received very little support. The new care coordinator allocated to Neil never met him. Neil was discharged from the Care Programme Approach (CPA) in July 2013.[6]
4.15 Neil had regular contact with staff at the Clozapine Clinic where he went every six weeks for a blood test. When the clinic changed its location from St Stephens to Hellesdon around October 2013, Neil had an hours walk each way. His bicycle had a flat tyre and Neil not knowing how to repair it and stopped using it.
4.16 Neil’s physical appearance changed from 2012. He was still visiting his sister and her family every week but she noticed that he was unkempt and there was ‘a distinct lack of personal hygiene’. His sister said, ‘He sort of gave up on himself.’ She thought that he was getting malnourished, ‘The only decent meal he got was with us once a week.’
4.17 Following Neil’s death his sister visited the flat and was shocked to see how Neil had been living. Her contact had been through his weekly visits to her family home and so she was unaware of the decline in the appearance of Neil’s home. She says, ‘Literally everything was covered in cobwebs. I opened his chest of drawers. The clothes were in neat little piles but he hadn’t taken them out for months’. There were cobwebs behind the curtains; Neil kept them closed because he thought the neighbours were spying on him. His mattress and sheets were dirty. There were unopened tins and frozen meals that his family had bought him years ago. The fridge had nothing in it but cans of Coke.
4.18 His brother in law said ‘Apart from going up to the local Co-op to get his sandwiches at lunchtime and maybe taking a packet of crisps and a sausage roll into his neighbour for company, he would spend 23 hours a day sleeping on his bed. His home became his prison.’
4.19 Neil’s sister and brother-in-law believe that Neil was incapable of making decisions about his care as he did not understand the consequences of these decisions on his health and wellbeing. They feel that the lack of care and support Neil received in the two years before his death led him to be in a situation where he did not have the mental, emotional and physical resilience or professional support to manage when things reached a crisis point in January 2014.
[6] Letter to GP from Speciality doctor dated 26th July 2013
Narrative chronology of pivotal events
5.1 The following narrative describes pivotal events between 2005 when Neil was first diagnosed with paranoid schizophrenia to his death in January 2014 . An integrated chronology with details of agencies involvement with Neil is provided separately. Comments in italics are the author’s observations.
2005 – 2006
5.2 30th August 2005 – GP referred Neil for a Mental Health Act assessment as he was aggressive at home towards his mother. He was subsequently detained to Hellesdon Hospital under Section 2 of The Mental Health Act 1983
5.3 31st August 2005 – Neil absconded from the ward and made his way back to his mother’s address. He agreed to return to the ward. This incident unnerved Neil’s mother and concerns were expressed by his sister about any proposal for him to return to their mother’s address.
5.4 9th September 2005 – Ward round with Neil and family present. Housing application, gym, Occupational Therapy and Meridean East referrals discussed and actioned. The family met with a psychiatrist who gave a full explanation of Neil’s diagnosis with Neil’s consent. This came as a shock to the family ‘ We were totally unprepared. We thought, what on earth does that mean?’ [7] Despite professionals view that a full explanation was given the family did not feel that they were given the time and information that they needed, to help them understand Neil’s condition.[8]
5.5 20th September 2005– Neil had a further 1:1 with OT (also seen on the 9th Sept but was not well enough to undertake a formal assessment). Neil stated that he did not want an OT assessment and was able to self-care, but ‘not with eyes watching me.’
5.6 1st September 2005– Referred to the Emergency Intervention Team (EIT) for a care co-ordinator to be identified. This is marked as not being received until 30/9/2005.
5.7 28th September 2005- Ward round with Mr Neil Jewell and family. Discharge arrangements discussed. CRHT to support Mr Jewell in community. CPA review booked for 3 wks.
[7] Sister from transcribed interview notes
[8] ‘The wider picture surrounding Neil’s care’ – prepared by Neil’s sister
5.8 3rd October 2005 – Neil turned up at his mother’s house again. On return to the ward Neil agreed to see a nurse therapist. A referral was made to adult safeguarding on behalf of Neil’s mother.
5.9 4th October 2005- Ward round; family not present. Neil informed of side effects of medication. Discharge arrangements discussed including; accommodation (B&B), appointment with community psych nurse, Care Plan Approach (CPA) review and EIS referral.
5.10 Prior to discharge – Attended therapy sessions. Was assisted to complete benefit forms and a housing application (with Julian Housing support). Neil was seen by the Community Rehabilitation Team (9/10/05). He refused their support but agreed that he would see them if he needed to.
5.11 10th October 2005– Neil was discharged to Bed and breakfast accommodation. Neil’s family had raised concerns regarding discharge arrangements [9]. Neil did not have an OT assessment prior to discharge and had not been allocated a care coordinator.
5.12 18th October 2005– Readmitted under Section 3 following overdose of Olanzepine. Neil admitted to being non compliant with medication, unhappy in the bed and breakfast accommodation and feeling hopeless for the future.
5.13 Following readmission – The Emergency Intervention Team accepted the referral (dated 1/9/2005) on the 3rd November and confirmed a care coordinator on 10th November. An OT assessment was carried out on the 16th December. It concluded that although self-caring Neil would need support and encouragement to enhance existing skills e.g. cooking.
2006- 2007
5.14 Neil remained in hospital until 13th February 2006 when he was discharged to a supported living unit under the remit of Julian Housing. Whilst resident at the unit Neil was regularly reviewed and his needs assessed. His family were invited to the review meetings as and when Neil requested it. Neil was under the care of the Emergency Intervention Team at this time and had an allocated Care Coordinator in line with his Care Programme Approach status. Whilst at the supported living unit Neil progressed with working towards achieving employment and reinforcing self-care activities.
2007 – 2008
5.15 May 2007 Neil moved into a council flat.
5.16 8th June 2007– Neil met with Disability Employment Adviser to discuss help and support available on a voluntary basis from DWP. Referred to Meridian East to take part in Work Step (Movement towards work) programme. At this time. Neil was not required to take part in any mandatory work activity.
[9] Letters to GP from sister dated 29th March 2005 and 22nd August 2005.
The decision to refer to Meridian East was taken jointly with Mr Neil and his disability employment advisor.
5.17 . Between 1st May and 18th June 2007 – Neil underwent three reviews with the multi-disciplinary team this included; Julian Housing, EIT and Meridian East [10].
5.18 Neil’s sister continued to raise concerns about his ability to live independently [11]. The NSFT IMR states that these concerns were balanced against Neil’s basic human rights to a private life under the least restrictions to keep him and others safe.
5.19 Neil’s sister said [12], ‘Their ethos of managing mental health patients was – people have choices. But the point was, he was a paranoid schizophrenic he wasn’t able to make a balanced judgment of things. He had not had any life experiences to be able to do that’. His brother-in-law adds, ‘This brings us to one of our frustrations, that people who have studied the mind and human nature, psychiatrists if you like, still couldn’t understand how Neil thought and behaved and what he actually needed. His inability to make those decisions and choices. Somebody who was only too pleased to say what other people wanted to hear. They gave him choices and they are people who in my view should have known better – that he couldn’t make choices’.
2008- 2009
5.20 Employment – Neil successfully completed the Work Step Programme with Meridian East. At that time Neil agreed that he would look with them for warehouse work. In May he was due to start a job but Neil’s sister contacted NSFT to let them know Neil had concerns. A social worker visited Neil at home to discuss these concerns. As a result a referral was made to a befriending service on 21st May. A work placement was scheduled with Tesco in August. On 7th October Neil passes a forklift truck exam. However, despite these opportunities Neil told his social worker on the 12th November that he no longer wanted to get a job.
5.21 Neil’s brother-in-law describes this period when Neil was being supported by a Meridian East worker to find work. ‘Nobody understood, even when he had the other organisation Meridian East. You know he quite enjoyed going out with the chap. They would go out for an afternoon. Perhaps go out for a coffee somewhere. Go out for a walk. That was fine. It was company but at the bottom of it – he would set up various interviews for Neil. He was frightened of going into work because of his circumstances. He was bullied. He couldn’t deal with difficult situations’.
5.22 1st July 2008 – Neil called the Recovery team leader to say he had taken an overdose of Venlafaxine (antidepressant) and Paracetamol. Paramedics were called but Neil did not go to hospital as he said that he was fine. He agreed to attend an appointment with the Recovery team the next day.
[10] NSFT IMR
[11] CPA review refers to a letter from Neil’s sister dated 6/9/2007
[12] Transcribed interview notes.
5.23 1st August 2008 – Neil attended the Recovery team base. He expressed concerns about his neighbours as he believed they were being hostile towards him. At this time Neil’s care coordinator was on leave and Neil did not want to see anyone else.
2009- 2010
5.24 3rd February 2009- Neil attended accident and emergency after taking an overdose. Neil was experiencing an increase in auditory hallucinations and was paranoid about his neighbours. A medical review took place two days after this incident and this was followed by a CPA review a week later. As a result, medication was increased, support offered with his benefit claim, the befriender referral was followed up and it was agreed that Neil would receive regular support from a community support worker. Neil was given the contact number for the Crisis Resolution and Home Treatment (CRHT) Team if he experienced crisis out of hours.
5.25 March 2009 – Neil’s symptoms worsened as he experienced an increase in auditory hallucinations and Clozapine was prescribed. In May 2009 Neil was admitted for 16 days for Clozapine tritation to enable close monitoring of his blood pressure and response to the Clozapine.
5.26 Apart from a short period of non-compliance with medication in June which was picked up quickly by the community support worker and action taken to re-titrate, Neil improved in health and wellbeing. In August 2009 Neil had a successful camping trip with friends and planned a second one. He was enjoying cycling and attending a coffee club. During this period Neil was being seen weekly by the community support worker. The community support worker noted that Neil had been told about the need for regular meals and the impact of not eating and drinking on medication. In October 2009 it was decided that due to the stability of his blood results Neil would be seen at the Clozapine clinic rather than the community mental health team base.
2010- 2011
5.27 10th Feb 2010 – GP records noted he had not been collecting his repeat meds for several weeks but then a few weeks later started to collect them again. [13] This was the anti depressant Venlafaxine which Neil collected weekly from the GP practice. This is the 3rd time that non-compliance with medication is mentioned in the chronology see also 5.10 (October 2005) and 5.25 (June 2009 – non compliance in taking clozapine).
5.28 Jan – Feb 2010 – Neil’s mental health and wellbeing was poor in the first part of this year. He was still being seen weekly by his community support worker but was neglecting to care for himself. He was sleeping in his clothes and not washing, so personal hygiene was poor and he was rarely leaving his flat. Neil’s medical review was brought forward. Neil said he was feeling low due to the death of a neighbour. His anti depressant Venlafaxine was increased. The GP report 5.27 shows that Neil had not been collecting his prescription (Venlafaxine).
5.29 May 2010 –The burglary of a neighbouring flat and a blocked sewerage reinforced Neil’s anxiety and paranoia about leaving his flat unattended. Norwich City Council housing has confirmed that the blocked sewerage was reported and repaired. Norfolk police confirmed that there had been a burglary in Neil’s road at this time.
5.30 3rd June 2010 – Medical review. Seen by Consultant Psychiatrist and Community Support Worker. Plan to increase Clozapine and decrease Venlafaxine introduce Hyoscine kwells (travel sickness medication?) and review in 2 months.
5.31 July 2010 – The Community Support Worker continued to work closely with Neil. He helped to make the flat secure to reduce Neil’s anxiety and took him on another camping trip. Unfortunately Neil got an allergic reaction whilst on holiday and had to return early.
5.32 The community support worker attended a medical review with Neil on the 29th July 2010. No contact with Neil was recorded after this date. It is not clear from the chronology why the weekly visits from a community support worker discontinued. However, the IMR states that it was ‘as a result of the ‘cost improvement programme’ within the trust, which had led to the community support worker taking redundancy’.[14]
2011- 2012
5.33 16th March 2011 – Telephone call from CMHN 2 to inform Neil that she was his new Care coordinator. Neil was seen once by this Care coordinator on the 4th April 2011. On the 8th August 2011 Neil was informed by telephone that his care coordinator had changed again. Neil was seen by this new care coordinator and a community mental health nurse on the 5th September 2011.
2012- 2013
5.34 Reassessment for benefits claims – Neil had been receiving Incapacity and benefit income support, this allowance ended in Feb 2012 (Welfare reform bill) and was replaced with the ESA allowance. As part of this process Neil attended a work capacity assessment and an independent decision maker determined that Neil had limited capacity for work and would therefore continue to receive payments at the same rate. However, he was required to attend three monthly interviews at the Job Centre.[15]
[14] NSFT IMR
[15] DWP IMR and email response to questions raised by the SAR overview report writer.
5.35 6th June 2012 – Interview with advisor at Norwich Job centre. It was noted that Neil’s mood appeared to have dropped. Neil reported that he continued to live alone and had contact with family on Mondays, but no longer had a support worker and felt he had limited social contact. His medication was supplied by repeat prescription, so he was not having regular medical checks. Neil stated that his mood was more negative, and was reluctant to travel too far from home, by bike.
5.36 25th June 2012- CPA review; CP 1 and SW 1’s team leader TL1 present; appeared to be ‘doing well’, no activities, self care ‘ok’, concordant with medication, no symptoms of low mood. Plan; wean off Venlafaxine, see in 6 months. Neil had not seen a Care coordinator, Community Support Worker or a medic for 9 months prior to this appointment. It is not clear what the rationale was for ‘doing well’. No evidence of relatives being involved in this review’.
5.37 13th July 2012– A letter is sent to Neil’s GP to say that Neil would be coming off the anti depressant Venlafaxine over the course of two weeks. The speciality doctor at St Stephen’s Road says in this letter, ‘Neil continues to do well with no current psychotic symptoms, but he continues to live in an impoverished environment with no work or social linked activities. It seems to me that he is quite happy to leave things that way.’ From that date Neil would no longer visit the GP practice every Monday to collect his prescriptions.
2013 – 2014
5.38 18th July 2013 – CPA review with CP 2 and SW 1; noted ‘good self care’, concordant with medication, admitted to drinking 3-4 cans of lager daily. Discharged from CPA. Plan; continue on medication, review in a year, Care Coordinator to continue to review. The staff present CP2 and SW1 did not know Neil well and his family did not attend this review
5.39 Reassessment for benefits claim –On the 13th August 2013 a decision was made that Neil had limited capacity. Neil was awarded Employment Support Allowance (ESA) plus a support component and was paid arrears. Neil was attending three monthly interviews in 2013. The compliance officer who interviewed Neil had experience of working with customers with complex mental health needs. DWP say that support would have been offered, including advocacy support, if it was felt that Neil was having any difficulty in participating in the interview or understanding what was being said. The compliance officer understood Neil’s limitations but did not consider him to be having difficulty with the interviews. Neil was asked for bank statements in December 2013 and provided these to the Norwich Job Centre.[16] Neil’s family remember that he was very anxious about interviews with the compliance officer. ‘He was visibly shaking when he talked about the interviews and was not sleeping’.
[16] Email response from DWP to questions raised by SAR overview report writer.
5.40 2nd December 2013– Neil attended the Clozapine Clinic at Hellesdon and received one months supply of Clozapine to last from 02/12/13 to 13/01/14. [17] Neil’s family accept that records show Neil received this medication. However, they could not find the medication in his flat and point out that Neil did not have the ability to be deceitful. He has in the past admitted when he has not taken medication. We may never know why Neil did not take his medication. The evidence suggests that Neil had sufficient medication but Neil’s family’s knowledge of Neil suggests that there may be other circumstances that are not known.
2014 January
5.41 6th January 2014 – Neil walked to the Clozapine Clinic to tell them that he had not taken medication for four days and had diarrhea and vomiting. The clinic contacted a duty worker at the CMHT base. Neil’s new care coordinator got back in contact with the clinic and made arrangements for Neil to be admitted for re-titration onto Clozapine. As there were no available inpatient beds it was agreed that Neil would be admitted to Hamilton House on the 7th January 2014 (a community care home).
5.42 Neil visited his sister and family that evening as was usual on a Monday evening. Neil’s sister and brother-in-law recall, ‘ He was very agitated. We knew straight away. His eyes were glassy. He was all over the place. How did they let him go home in that state?’ Neil was very worried about getting to Hamilton House the next day. His sister explained that Neil didn’t know how he was going to get there. ‘We had several calls (from Neil) late that night and the early hours of the morning. He had no idea what the time was. It was as though he had been awake for days. His brain was just not switching off. His body was not stopping to give him some sort of break.’
5.43 A referral was made to and accepted by Hamilton House. A risk assessment dated 6/1/2014, a letter with the outcome of a CPA meeting held 18/7/2013 and an explanation that the Crisis Resolution Home Treatment (CRHT) Team would support Hamilton House re-titrate as stated in the plan (page 11) was sent [18].
5.44 7th January 2014- Neil waited at home for transport to Hamilton House. He called the clinic and eventually (late morning) was collected by taxi and accompanied by the clinical team lead and another member of staff from the CRHT team to Hamilton House. The CRHT team reported that Neil was observed to be thought blocked and anxious. He kept on apologizing for the inconvenience. Neil said that he had not eaten since the previous day when he was on Waveney ward and was getting stomach cramps. The CRHT team gave Hamilton House directions on re-tritation and told them that they could contact the CRHT team if required. An assessment was made by the CRHT team that there was no current role for input whilst Neil was at Hamilton House and they therefore did not take him on for home treatment [19]. This was communicated to the GP by letter but not to Hamilton House.
[17] Statement Pharmacy technician Operation Madeley S25A and copy from distribution log book D158
[18] Prime Life IMR
5.45 8th January 2014– Neil eating and drinking, vital signs (pulse and temperature) checked. He phoned the the CRHT team as he was agitated but they had trouble understanding him. Neil settled and slept well.
5.46 9th January 2014– Neil took himself to the staff office on waking. He was distressed as he was experiencing a high level of auditory hallucinations. His speech pattern was described as ‘word salad’. The CRHT team was contacted and they prescribed Lorazepam (a benzodiazepine, used as a sedative to reduce agitation). His vital signs (pulse and temperature) were checked. Neil settled after taking the Lorazepam and ate at mealtimes behaving appropriately.
5.47 During the night Neil became very disturbed, shouting and banging walls and doors. The CRHT team were contacted but they recommended that the home management team were contacted in the morning.
5.48 10th January 2014– 06.15 The police were called with a request to assist with a potentially violent patient. Two police officers attended 10 minutes later. They found Neil to be tense, angry and upset. He appeared to be having auditory hallucinations but was not physically violent. The nurse at Hamilton House explained that he had been verbally aggressive. Neil had returned peacefully to his room when the police left.
5.49 At the same time as the police visit Hamilton House contacted the CRHT team who suggested that they contact social services for an urgent Mental Health Act (MHA) assessment. The Emergency Duty Team (EDT) received a request for a MHA assessment at 07.30. The Duty Social Worker confirmed that she would liaise with the CHRT team so that a MHA assessment could be arranged. The request for a MHA assessment was passed to the day shift at 9.00am.
5.50 The CRHT team in discussion with Neil’s care coordinator prescribed Haloperidol (an anti psychotic medication) in addition to Lorazepam. As there were no in-patient beds in the area the CRHT team felt that if Neil were to have a long journey that it might disturb him more and asked Hamilton House if they could manage Neil if he was better supported with medication. Hamilton House agreed and increased their staffing levels to manage Neil during the night. Neither the CRHT team worker or the care coordinator knew Neil and they did not see him before making this recommendation. The MHA assessment was not followed through as a result of this intervention.
5.51 Neil’s sister visited that evening. She was shocked and upset to find her brother in such a disturbed state of mind. She said that ‘he did not know I was there and sadly this was to be the last time I saw him alive.’ Neil was saying his brother-in-law’s name and his sister told staff that she thought Neil’s recent involvement with a welfare benefit officer, something he had been discussing with his brother-in-law ,had troubled him.
[19] CRHT assessment dated 7/10/2013 sent to GP 8/1/2014
5.52 11th January 2014 – 02.00 Neil was banging on doors, had incoherent speech and took off his clothes, wandering naked. Hamilton House contacted the Emergency Duty Team (EDT) and requested a MHA assessment. They took away a couple of belts, a razor and shoe laces from his room as they were concerned Neil would self harm.
5.53 03.25 The Approved Mental Health Practitioner (AMHP) contacted the on call EDT duty manager and was advised that Neil’s referral should take priority over any others.
5.54 05.40 East of England Ambulance were called with a request to transport a patient from Hamilton House to Wedgewood House (West Suffolk) within four hours. If entries are correct this was before Neil had been sectioned but it is likely that 5.49 below had taken place and was recorded at 05.55.
5.55 05.55 the AMHP and two doctors attended Hamilton House to carry out a MHA assessment. Neil was detained under section 2 of the MHA and Neil’s sister was informed by telephone. A call was made to the police requesting that officers attend Hamilton House to prevent Neil absconding whilst awaiting an ambulance to transport him to Southgate Ward, (West Suffolk). The assessing doctors advised the AMHP that Neil could be managed in an open ward.
5.56 06.10 Two police officers arrived at Hamilton House. They waited in a lounge area for 10 minutes and were then called urgently to Neil’s room. Neil was naked rocking backwards and forwards and chanting. His room was in disarray and the mattress had been upturned from the bed. There was blood on the window sill. A member of staff expressed concern that there were springs in the mattress and Neil could use these to self harm. A police officer took hold of Neil’s left arm to pull him away from the mattress. Neil began to resist. Both police officers then restrained Neil on the floor. When Neil continued to resist he was handcuffed (hands behind his back) and placed on his side.
5.57 The AMHP called the East of England Ambulance Service requesting an estimated time of arrival and requesting the journey was prioritized. He called Wedgewood House shortly before Neil left advising them that Neil would need sedating and assessing immediately on arrival. Wedgewood House questioned whether a Psychiatric Intensive Care Unit (PICU) bed was more appropriate. The AMHP agreed but was told there were none available at that time.
5.58 Shortly after 07.00 Two more police officers arrived to assist their colleagues. Their arrival was followed a few minutes later by an ambulance. The officers used Emergency Restraint Belts (ERBs) to control Neil. One was placed around the upper half of his body, the other around his legs. Neil was lifted onto a portable stretcher and placed in the ambulance on a secured stretcher bed. The ambulance left Hamilton House at 07.21 and arrived at Southgate Ward, Wedgewood House at 08.42. Neil remained handcuffed and restrained with straps throughout the journey. He was lying prone. Police travelled with Neil. The ambulance used a blue light.
5.59 On arrival at Wedgewood House Neil was placed in a Section 136 suite because the low stimulus area that would have been more appropriate was not available. At 10.45 a decision was made to seclude Neil in a locked room with observations every 15 minutes.
5.60 18.12 Neil was transferred to an Ipswich PICU bed, transported in a secure private ambulance (UK SAS). Neil was not restrained for this journey as the layout of the vehicle allows for the escort to sit in the back close to the cell to observe the patient and ensure that their safety is maintained throughout the journey. The journey was carried out at normal road speed with no blue lights or sirens.
5.61 18.50 Neil arrived at (Lark Ward). He was placed in seclusion again to avoid restraining him as he had injuries to his arms and back from restraint straps and handcuffs and was still very agitated. Medical reviews at 19.30 and 21.30.
5.62 12th January 2014– Neil remained in seclusion where he was observed between 09.00 and 16.16 to be moving around the room, lying on a mattress and moving his arms and legs. When observed at 16.30 Neil had not moved since the last observation at 16.16. The staff member called another member of staff and together they entered the room. Neil was unresponsive; cardio pulmonary resuscitation (CPR) commenced and emergency services were called.
5.63 17.19 – Neil was taken by ambulance to the emergency department of Ipswich Hospital where he was treated with three cycles of CPR and two adrenalin injections. He was then taken to critical care where he was put on a ventilator.
5.64 17th January 2014– Neurophysiological investigations and tests found that Neil had irreversible brain damage. A decision was made with his family to discontinue the life support system and Neil died at 20.18.
6.0 Analysis
6.1 There are examples of notable practice as well as areas where partners could work together more effectively. The notable practice is described first. .
6.2 Response to crisis Between 2007 and 2011 Neil’s mental health fluctuated and he reached a crisis point on more than one occasion. At this time he was well supported and the care team around him responded quickly and appropriately. See table one.
Table one
July 2008 Neil called the Recovery Team Leader to say he had taken took an overdose of Venlafaxine and Paracetomel. Paramedics were called but Neil did not want to go to the hospital. Instead arrangements were made and followed through for him to attend the Recovery Team base the next day.
February 2009 Neil attended accident and emergency after taking an overdose. He was experiencing an increase in auditory hallucinations and paranoia about his neighbours A medical review took place two days after this incident and was followed up with a CPA review a week later. Neil was given the number of the Crisis Resolution and Home Treatment Team if he experienced crisis again out of normal work hours.
February 2010 Neil’s Community Support Worker noticed that Neil was neglecting to care for himself. Neil told him that he was feeling low due to the recent death of a neighbour. Neil’s medical review was brought forward and his anti depressant increased.
6.3 Between 2007 and 2011 Neil was supported by two different support workers and a Meridan East worker, all of whom who spent time getting to know Neil, his strengths and interests as well as his limitations. They encouraged him to try new things and helped to build his confidence and self esteem.
6.4 When Neil’s mother expressed her fear that Neil would be violent towards her in 2005 a referral was made on her behalf to the Norfolk Safeguarding Adults team.
6.5 Neil was transported in a secure private ambulance on the 11th January from Wedgewood House to Ipswich Hospital when he was moved to a PICU bed.
This meant that he did not have to be physically restrained. He was kept safe and observed with the least restrictive intervention. The ambulance did not use a blue light or a siren and so it was a calm and well managed journey.
6.6 Neil’s health was monitored by the general practice and mental health trust in line with the National Institute for Excellence (NICE) guidelines on monitoring for cardio metabolic risk factors.
6.7 This analysis draws on information gathered through IMRs and other reports to identify lessons learnt in how professionals and services work together. These have been grouped under five headings:
- Self-neglect
- Person centred care planning
- Information sharing and joint decision making
- Use of control and restraint
- Attention to physical health needs
6.8 The following issues are picked up under one or more of these headings:
- Relationship between professionals, Neil and his family
- Identification and management of risk
- Review of whether the correct processes, protocols and procedures were followed and required standards were met.
6.9 This review also identified a number of agency specific issues. These are being dealt with by individual agencies and are outside the scope of this review. The agencies listed in 3.6 have produced Individual Management Reviews (IMRs) and action plans. The Suffolk and Norfolk Safeguarding Adult Boards will monitor implementation of the action plans. A number of actions have already taken place ahead of this report being completed.
7.0 Self-neglect
7.1 This section explores whether the right balance was achieved between recognizing Neil’s right to make life style choices that resulted in self neglect and a duty of care by professionals to safeguard Neil from harming himself through self neglect.
7.2 Self-neglect is common in people living with paranoid schizophrenia. Some of the symptoms of schizophrenia include social withdrawal, a deterioration of personal hygiene, neglecting appearance, a lack of interest and enthusiasm, apathy and a general disinterest in life [20].
[20] http://www.helpguide.org/articles/schizophrenia/schizophrenia-signs-typesand-causes.htm accessed 30/04/15
7.3 Reports from 2009 onwards show that Neil was neglecting to care for himself. He had poor personal hygiene, and was wearing the same clothes day and night for a week [21]. He was also neglecting to eat properly and maintain a healthy lifestyle. Table two below shows entries in his case records to this effect.
7.4 Table two Entries reporting self-neglect
3rd Feb 2009 Neil’s sister telephoned the community mental health nurse to register her concern that Neil was not eating and was losing weight. 30/6/2009 Seen at home – blood sample taken and physical observations. Information given re the impact of not eating and drinking properly on medication.
25th Jan 2010 Community support worker entry ‘Patient sleeping in his clothes and not washing. We discussed personal hygiene’.
21st April 2010 Seen at home by community support worker. Neil not leaving his flat and sleeping in his clothes, resistant to addressing this
2nd Feb 2010 Telephone call from sister who is concerned about Neil’s deteriorating mental health, poor hygiene, lack of activity and being withdrawn. Reassurance was given that these matters were being discussed with Neil and his medical review would be brought forward.
15th Feb 2010 Neil was seen at home by his community support worker. A record is made that personal hygiene was poor and Neil was disinterested in any activities outside of the house.
8th June 2010 Neil was seen at home by his community support worker and care coordinator. They discussed with him his lack of participation in activities, poor hygiene and issues with auditory hallucinations. They agreed a plan to make his flat secure so that he would feel safe leaving his flat. He had been worried about a recent burglary in the area.
7.5 Neil’s sister was particularly concerned about his neglect to eat properly. He lived off sandwiches rather than prepare himself a meal. Neil’s sister and mother had bought him some ready meals to prepare in the microwave when they could see that he was struggling to prepare a simple meal such as a cold quiche and salad. However, when Neil was admitted to hospital in 2014 they found the ready meals ‘welded in the freezer’ untouched, they were dated 2010.
7.6 An OT report dated 16th December 2005 assessed Neil to have a ‘good understanding of nutrition and what constitutes a balanced diet. Neil was able to carry out transactions (shopping) independently and stay within budget’.
[21] NSFT risk assessment 2012
It went on to say, ‘This assessment demonstrates that Neil would benefit from opportunities to practice cooking skills further with support to build on these skills. He would also benefit from support and encouragement with other daily activities such as cleaning and providing structure to his day.’
7.7 Whilst Neil might have had the ability to prepare a meal in 2005 this was clearly not the case in 2010. Neil did not have any further OT assessments; neither did he have any support and encouragement to develop his daily living skills as recommended in the OT report.
7.8 Neil’s sister registered her concern regarding his loss of weight and poor diet on at least two occasions (table two above). His diet of sandwiches could not have had much nutritional value, however GP records show that his body mass index whilst showing a loss of weight in 2012 and 2013 remains within healthy limits (table three).
7.9 Table three Record of Neil’s weight
Body mass index
22/05/07 01/03/12 23/01/13 12/03/13 31/10/13
Height (m) 1.8 1.8 1.8 1.8 1.8 Weight (kg) 94 74 90 84 BMI (kg/m) 27.47 22.84 27.78 25.93
Source GP practice medical records
Healthy BMI is 18.5 to 24.9 Underweight if BMI is less than 18.5 Overweight if BMI is between 25 and 29.9
7.10 Neil’s sister felt angry that her brother was left to care for himself without any support. She felt that he should have been offered a more sheltered environment than the council flat in which he was living. ‘He needed a safety blanket around him.’ They were frustrated that staff kept on repeating that Neil had to make his own choices about his lifestyle and where he lived. ‘Their ethos of managing mental health patients was – people have choices. But the point was, he was a paranoid schizophrenic he wasn’t able to make a balanced judgment of things. He had not had any life experiences to be able to do that’. They felt that he would have had a much better quality of life and may never have ended up in the crisis he was in had he had the support around him that he needed.
7.11 There are two parts to this argument, whether Neil had the mental capacity to make the lifestyle choices that he did and whether he received the support and care that he needed to live independently. Each of these issues is addressed below.
7.12 There are some similarities to a case that was taken to the Local Government Ombudsman and Health Service Ombudsman (May 2014). The complaint was from the sister of a man with paranoid schizophrenia who was living in a flat in squalor. He had poor self-care and an inadequate diet. It was argued that failure to carry out a proper capacity assessment of his ability to make decisions about managing food and looking after himself had resulted in him being malnourished.
7.13 The Mental Capacity Act 2005 and the accompanying code of practice say that a person should be presumed to have capacity unless it is otherwise established that they lack capacity. This decision is one of professional judgment.
7.14 Mental capacity means that the person is able to weigh up the information and is able to understand the consequences of decisions and actions as well as the ability to implement those actions. Neil’s sister argues that Neil was not able to weigh up information and understand the consequences of his choices and actions. She makes the point that Neil would not understand the impact of not taking his medication. Non compliance with medication is a form of self neglect and although it was rare for Neil, there are three reported occasions when this happened prior to January 2014 (see 5.27 narrative chronology).
7.15 A mental capacity assessment was not carried out to determine whether or not Neil lacked capacity to make the choices he did regarding where he lived and how he lived. Whilst a professional judgment might have been made of presumed capacity, this should have been supported by a risk assessment and plan that took into account his sister’s views, Neil’s life history, the impact this might have upon his decision making and the support that could be provided to Neil to minimize any risk to his health and well-being as a result of his lifestyle choices.
7.16 Neil may or may not have had the capacity to make informed decisions about his lifestyle. Braye et al (March 2015) describe the competing moral imperatives of ‘a respect for autonomy and self-determination’ and that of ‘a duty of care and promotion of dignity’. A well informed risk assessment and plan could have provided some assurance of getting this balance right.
7.17 Supporting people who self neglect to live a healthy lifestyle when they are not motivated to do so presents a challenge for staff. It is only in recent years that self neglect has been recognised as an adult safeguarding issue (The Care Act 2014). The Social Care Institute for Excellence guidance (Braye March 2015) for professionals working with people who self neglect recommends care staff:
- Build a relationship of trust with the person over a period of time and at the person’s own pace
- Find the whole person and understand their life history
- Take account of the person’s mental capacity to make self care decisions
- Be open and honest about risks and options
- Multi agency working
- Creative and flexible interventions
7.18 Between 2007 and 2012 Neil had regular contact with a Community Support Worker that he knew well. Neil’s sister describes how the regular contact with a care worker that he knew increased Neil’s confidence and encouraged him to participate in social activities.[22]
7.19 Table two shows that care staff discussed personal hygiene and a healthy lifestyle, including a balanced diet with Neil. There are similar entries in notes from CPA meetings. However, this seems to be the only intervention and it does not seem to have had any impact in changing Neil’s behavior.
7.20 Braye et al (2015) recommend that a hands on approach is needed seeking opportunities for agreement to do things that will make a small difference while negotiating bigger things and deciding with others when risks are so great that some intervention must take place.
7.21 Neil’s Community Support Worker did agree with Neil that they would secure his flat to encourage him to participate in social activities (table two above). This was a sensible and creative intervention. However, perhaps more could have been done with hindsight to discuss options with Neil. For example, his sister said that he could have paid for a home help to clean his flat. Neil enjoyed eating his meal with others, he visited his sister once a week to share an evening meal and visited a neighbour to eat his sandwich with him. Neil attended a weekly coffee club, maybe he could have attended a lunch group or paid to eat a meal in a local facility on a regular basis. There is nothing to suggest that any options were discussed with Neil.
8.0 Care Plan Approach and person-centred care
8.1 This section identifies what worked well in care co-ordination and CPA and where things did not work so well.
8.2 A person centred approach to care has been the ethos for mental health services since the National Service Framework for Mental Health Services was published in 1999. It means services that are organised around the person so that they are able to respond to the needs and wishes of the person in a coordinated way. The Care Programme Approach (CPA) is a national system for the way in which mental healthcare is planned and delivered. It means that a person should be allocated a care coordinator, have multi-disciplinary care planning and review meetings and a written care plan. A person who meets the CPA criteria should have regular contact with a care coordinator. The care coordinator should fully assess the person’s needs with a multi professional team taking into account;
- Employment, training or education
- Personal circumstances including family and carers
- Social needs
- Physical health
- Potential risks
- Problems with drugs or alcohol
[22] Transcribed interview notes
8.3 Department of Health guidance (DH March 2008) says, ‘Make sure that service users and their carers are partners in the planning, development and delivery of their care. They need to be involved in the process from the start.’
8.4 National Institute for Clinical Excellence (NICE) guidance (Dec 2011) states the importance of discussing with the person using mental health services if and how they want their family or carers to be involved in their care. It goes on to say that such discussions should take place at intervals to take account of any changes in circumstances, and should not happen only once.
8.5 Between November 2005 and April 2009 Neil had a care coordinator and had regular CPA reviews. Neil’s family were invited to these reviews as and when it was agreed with Neil (see table four below). Neil did not always want his family to attend CPA reviews and staff respected this. It is understood that sometimes issues may be discussed of a personal nature that a person does not want shared with their family. However the family needs to be kept informed and involved in other ways as agreed with the person. Involvement with the family is not consistent in Neil’s care.
8.6 Table four CPA reviews
22/11/2005 CPA review on ward family attended
20/12/2005 CPA review on ward
7/2/2006 CPA review on ward
7 /2/2006 & 13/2/2006 CPA review on ward (prior to discharge)
13/3/2006 CPA review – family attended 31/5/2006
CPA review in community (family only to be invited when agreed with Neil)
7/8/2006 CPA review in community – family invited but did not attend
7/2/2007 CPA review in community
23/5/2007 CPA review in community
18/6/2007 CPA review in community
26/9/2007 CPA review – Sister attended, letter from sister dated
06/09/2007 raising some concerns which were discussed at this meeting; handover between teams, risk to mother, self care, activity, dip in mood since moving into own flat.
14/1/2008 CPA review – transferred to Recovery Team CMHT
10/2/2009 CPA review – CP1; Meridean East worker, EIS3, CSW1, sister and mother. Doesn’t feel ready to work, sees CSW1 every 2 wks, explore further activities in the week, chase up Befriender referral. Meridean East no longer to be involved in view of Mr Jewell’s not being ready to go back to work.
28/7/2009 CPA review CP1, CSW1, CMHN1 and Mr Jewell. Doing well.
25/6/2012 CPA review; CP 1 and SW 1’s team leader TL1 present; appeared to be ‘doing well’, no activities, self care ‘ok’, concordant with medication, no symptoms of low mood. Plan; wean off
18/7/13 CPA review- discharge from CPA.
8.7 Care coordination appears to be good between November 2005 and July 2009. Consideration was given to Neil’s employment and his need for social interaction with reference made to a befriending scheme. It is unfortunate that despite several referrals to the befriending scheme this did not result in a service. The community staff attending the CPA reviews knew Neil well and were able to discuss care needs and wishes with Neil and his family (as and when they attended) in an informed way. This however was not always the case.
8.8 Neil was admitted to hospital under Section 2 of the Mental Health Act on the 30th August 2005 and discharged on the 10th October 2005 to a bed and breakfast. Although a referral was made to the Emergency Intervention Team (EIT) for a care coordinator to be identified the referral was not accepted until the 3rd November 2005 with a confirmed care coordinator allocated on the 10th November 2005.
8.9 Neil was discharged to a bed and breakfast on the 10th October 2005, despite his sister writing a letter to the GP and psychiatrist expressing the family’s concern that this was not appropriate accommodation for Neil and the risks it would present to his health and wellbeing. A referral was made to occupational therapy (OT) for an assessment of Neil’s daily living skills but his discharge took place before an assessment was carried out.
8.10 Neil was discharged without a well informed assessment of his needs, without considering the concerns of his family and without a care coordinator or CPA in place. This demonstrates poor discharge planning and poor practice in the planning and provision of aftercare. Had Neil been discharged following admission under Section 3 of the Mental Health Act this would have been a breach of statutory responsibilities as Section 117 of the Act states ‘aftercare services must be provided to patients who have been detained in hospital for treatment under Section 3.’ Neil was readmitted 8 days later under Section 3 after taking an overdose.
8.11 Between the 28th July 2009 and 25th June 2012 Neil did not have a CPA review. He did have medical reviews as shown below in table five.
8.12 Table five Medical reviews between July 2009 and June 2012
16/4/2009 Medical review; CP1, CMHN1, and Mr Neil Jewell, family not available (on holiday) so this meeting was not a CPA review as planned. Discussed process for change to Clozapine and side effects all discussed.
7/7/2009 Medical review
5/2/2010 Medical review
3/6/2010 Medical review – seen by Consultant Psychiatrist and community Support Worker
29/7/2010 Medical review This was the last review with the Community Support Worker that knew Neil well.
11/4/2011 Medical review
8.13 The Community Support Worker that knew Neil well had his last recorded contact with Neil on the 29th July 2010. After this medical review the weekly visits from a Community Support Worker appear to have stopped. There is nothing to indicate that Neil’s needs changed or to explain why this regular contact with a Community Support Worker came to an end. The NSFT IMR explains that this worker’s post was made redundant as a result of a cost improvement programme in the trust. However, Neil’s care plan should not change unless his CPA review identified a change in his care needs. If there was a change to his care plan this has not been documented and his sister was not made aware.
8.14 An entry dated the 5th September 2011 on the chronology, records a visit to Neil by his community mental health nurse and his new Care Coordinator. It says,’ ‘Neil is still not engaging in activities, continues to see family regularly, agreed to see his Care Coordinator as needed’. This does not meet the CPA requirement for a person receiving CPA to have regular contact with their Care Coordinator.
8.15 Neil was seen twice by a Care Coordinator in 2012, it was a different one each time as the Care Coordinator changed. When Neil had a CPA review in June 2012, he was not known to the social worker who had taken on the role of Care Co-ordinator and had not been seen by a Care Coordinator, Community Support Worker or medic for 9 months prior to the meeting. The CPA review reported that he was ‘doing well’ but this judgment seems ill informed. It is contradicted by the records of the Job Centre Advisor who says that Neil felt his mood was more negative and that he was having very little social contact since he no longer had a support worker and was not having regular health checks.
8.16 On the 18th July 2013 Neil had his last CPA review and a decision was taken to discharge him from CPA. A letter from his psychiatrist to his GP says that ‘it was revealed at the meeting that he is doing well for long periods of time.’ It also says, ‘He sleeps well, eats well and has good concentration.’ And ‘He admitted to drinking three to four pints of lager a day.’ This assessment does not fit with other records that show Neil was not eating well or the effects of social isolation on his mental health. The psychiatrist did not seem concerned that Neil was drinking three or four pints of lager a day, despite substance misuse being a high risk for people with schizophrenia. The letter says that his Care Coordinator ‘will continue to monitor him in the community.’ However, this same Care Coordinator says in a statement [23] ‘I did initially struggle to remember Neil as at that time my workload was around sixty-five to seventy at one time. Neil was an unassuming character who I had not too much involvement with as there was no need.’
8.17 Section 8.0 on self neglect stresses the importance of consistency in care workers so that they can build a trusting relationship with the person. Apart from his family and occasional contact with neighbours all of Neil’s social contact was with or through care workers. In July 2012 Neil’s prescription for anti depressants stopped and so he no longer had a reason to visit his GP practice once a week. He was no longer visiting the Community Mental Health Team base to collect his Clozapine as this changed to the Clozapine Clinic in 2009. Neil therefore only had contact with staff at the Clozapine Clinic from July 2012 and their role was limited to the monitoring of medication. Neil did not know who to contact when he needed additional support.
8.18 The letter to Neil’s GP regarding the decision to discharge him from CPA does not give a reasonable explanation as to why this decision was made. The mental health trust IMR states that Neil clearly met the criteria for CPA status.
8.19 Department of Health Guidance on CPA (DH 2008) states that when CPA is no longer needed that ‘a thorough risk assessment, with full user and carer involvement, should be undertaken before a decision is made that the CPA is no longer needed.’ Neil’s family were not involved in this decision and a risk assessment was not carried out. It warns against stopping CPA too early because a person appears stable and well.
8.20 The guidance goes on to say that CPA should not be withdrawn without:
- an appropriate review and handover (e.g. to the lead professional or GP)
- an exchange of appropriate information with all concerned, including carers
- plans for review, support and follow up, as appropriate
- a clear statement about the action to take, and who to contact, in the event of relapse or change with a potential negative impact on that person’s mental well-being.
[23] Statement S33 Operation Mandeley
8.21 The brief letter from the psychiatrist to the GP dated 26th July 2013 requesting the GP to ‘monitor his physical health annually as he is on antipsychotic medication’, that he (Neil) ‘will be followed up annually’ and ‘if there are any concerns he (Neil Jewell) is advised to contact us,’ does not meet with this requirement.
8.22 In 2013 Neil did not know who to contact when he experienced any difficulties or a decline in his mental health. He was not being seen by any health or social care professionals on a regular basis who could monitor his health and well-being. Despite his past history there was not a plan in place to monitor when Neil might need additional support, how he was to access it or how the multi professional team would respond to a crisis.
9.0 Information sharing and joint decision-making
9.1 This section addresses how information was shared between staff and agencies caring for Neil, the effectiveness of these systems and how information and intelligence on Neil’s past history, needs and wishes informed decision making.
9.2 Information was not shared between the Norfolk mental health service and Suffolk when Neil was transferred from Hamilton House to Wedgewood House on the 11th January 2014. Although these services are within the same hospital trust the information systems are not compatible and so information cannot be shared electronically. The medication sheets were not transferred with Neil and so staff had no information on medication on Neil’s admission to Wedgewood House or Lark ward the PICU bed where Neil was transferred later that day.
9.3 This presented a potential risk as Neil had been administered rapid tranquilisation drugs since the 9th January at Hamilton House. However, comments in the mental health trust IMR and chronology provide some assurance that the medication administered was within safe prescribing limits. See table six below.
9.4 Table six – Administration of medication 9th – 12th January 2014
10th January 15mgs Haloperidol (3x 5mgs) given and 2mgs Lorazepam (2x 1mg) given in 24hrs.
11th January Medication; 15 mgs (3x 5mgs) Haloperidol given PRN and 6 mgs Lorazepam (4x 1mg, 1x 2mgs) given PRN and 50mgs (1x 50mgs) Promethycine – in 24 hrs
12th January Haloperidol rapid tranq 10mg, oral 5mgs and 1mg Lorazepam rapid tranq received in total on 12/01/2014. Also given 1g of Paracetamol for bruising
9.5 Ward staff contacted Neil’s sister to get information on his medication. Although this highlights poor communication it did enable staff to manage the risk. Neil’s sister said, ‘ There seems to have been a total lack of communications right from the word go. No records were passed on. Computers do not talk to each other. I kept being asked even the very last day – What medication is he on? Everyone along the way kept asking about his medication’.
9.6 The lack of information when Neil was admitted to West Suffolk ward also meant that the risk assessment for his care was very poorly informed. The risk profile for Lark ward says, ‘Norfolk mental health services have been unable to provide information on this gentleman – they report that there is no meaningful information on their EPR (electronic patient record)’. The lack of a trust-wide patient record system has been picked up as a learning point in the mental health trust’s IMR.
9.7 The chronology highlighted opportunities where information might have been usefully shared between agencies. The GP’s records note that Neil had not been collecting his repeat medication for anti depressants on the 1st February 2010. At a medical review on the 5th February the consultant psychiatrist increased Neil’s anti depressants, as he had been feeling low in mood. It is possible that the drop in mood was as a result of non-compliance with his medication, but this information does not seem to have been shared.
9.8 The Norwich Job Centre Advisor was interviewing Neil every three months at a time when Neil had very little contact with any health and care professionals. The information that this advisor had on Neil’s health and wellbeing might have usefully informed Neil’s CPA review as the picture recorded on 25th June 2012 of ‘doing well’ is quite different from that described by the Job Centre Advisor on the 6th June. Likewise the Job Centre Advisor would have benefitted from having information on Neil from the mental health trust. An assessment was made that Neil did not need help or support in attending the interviews and responding to requests for information but his distress at the time of admission to Hamilton House suggests that this was causing him some anxiety.
9.9 Norwich City Council Housing Department were not involved in Neil’s care but could have fulfilled a valuable role. The Social Care Institute for Excellence say in their guide on safeguarding for housing staff (SCIE 2014) ‘Sharing and coordinating information on people with care and support needs who may be at risk of abuse and those who pose a risk cannot be under estimated.’ It is possible that Neil was experiencing financial abuse from his neighbours as his sister reports that they were taking advantage of his generosity. Neil’s vulnerability and history of self-neglect suggest that housing could have played a role in helping to prevent Neil’s situation deteriorating.
9.10 Sometimes a person might not appear to be at risk of abuse or neglect but when information is gathered from a number of organisations the risk of abuse or neglect is increased through the cumulative assessment. It is worth considering how partners such as the GP, housing provider, Job Centre and community and voluntary organisations share information and intelligence that might help the local authority identify when a person is at an increased risk of abuse or neglect.
9.11 The lack of information and intelligence to make an informed decision with the person and their family carers (when appropriate) has been highlighted earlier in the decision to discharge Neil to a bed and breakfast (8.10) and in discharging Neil from the Care Programme Approach (8.16). Poorly informed decision making is also apparent in the examples below.
9.12 A risk management plan was completed by his Care Co-ordinator when Neil presented himself at the Clozapine Clinic to report that he had not been taking his medication. Whilst it is good that a risk management plan was prepared it would have been more beneficial had it been a robust plan that addressed the risks of; delaying Neil’s admission to Hamilton House to the next day and admitting Neil to a care home rather than an in-patient bed.
9.13 The person completing the risk management plan did not know Neil. There is no past history about previous crisis and how these were managed. It does not identify Neil’s strengths or anything about him that might help the team to understand his needs and provide person centred support.
9.14 The plan recommends that Neil is admitted to Hamilton House the next day as an alternative to a hospital stay, for ‘re-titration of clozapine supported by CRHT’. This risk management plan does not identify any risks associated with this option. It does not offer any other options and neither does it address how the options were discussed with Neil or his sister.
9.15 The plan does say that Neil is to have contact with ‘mental health services so that Neil feels able to contact his care team to discuss any problems or concerns he may have.’ This is good, but when Neil tried to talk to the CRHT team on the 8th January from Hamilton House he did not get this support. An entry in the chronology says, ‘Neil had asked to speak to the Crisis Team 22.10 hrs which he did, although they were not able to fully understand all he was saying. He wishes to speak to his care team tomorrow’.
9.16 The plan says, ‘He appears emotionally labile, a little paranoid but was requesting help and entirely amenable to whatever intervention was suggested.’ In hindsight of what was to follow, this was the ideal opportunity to explore the options for intervention with Neil and his family, including where and when he was admitted for re-titration. The risk management plan did not identify the risks, the options or the discussions that were had with Neil and his family.
9.17 The role of the CRHT in supporting Neil at Hamilton House was not made clear in the risk management plan. The only specific action identified for the CRHT is for the CRHT team to see Neil the next day and transport him to Hamilton House and for the CRHT team to collect the clozapine on the morning of the 7th January.
9.18 A member of the CRHT wrote in a letter to the GP dated 8th January that ‘Following a referral from x (care co-ordinator) on 8th January, Neil was assessed by the Crisis Team and not taken on for home treatment.’ The assessment attached to this letter repeats the plan for re-titration at Hamilton House and says that, ‘Hamilton House are aware that they can contact CRHT if required, and there is no current role for CRHT input whilst at Hamilton House.’ This was not communicated to Hamilton House and so caused some frustration and confusion as staff at Hamilton House had expected greater involvement from the CRHT team in managing Neil’s care.
9.19 A referral was made to the Emergency Duty Team for a MHA assessment on the morning of the 10th January. Neil’s care co-ordinator and a member of the CRHT team made a decision without seeing Neil or knowing him well that the MHA assessment would not be carried out and that Hamilton House would manage ‘if he was better supported with medication.’ Hamilton House agreed and arranged for additional staff to cover the night shift. Again, with hindsight this decision was ill informed. It was not supported with a risk assessment or a well thought through plan. The rationale given was that ‘a long journey might disturb Neil more’. The potential risks of Neil becoming more agitated and how this would be managed, including the use of control and restraint beyond tranquilisation has not been documented.
9.20 The examples given of poorly informed and communicated decisions including:
- Neil’s discharge to a bed and breakfast
- Discharge from the Care Programme Approach
- Admission to Hamilton House (a Care Home) for treatment the next day rather than to an in-patient ward
- Not to carry out a MHA assessment when the request was first made by Hamilton House
- GP not communicating to the mental health trust that Neil had not collected his prescription.
It may have been the best options. However, these critical decisions were made without considering Neil’s past history, without consulting his family and without carrying out a robust well informed risk management plan that considered all of the options and set out agreed actions and the person responsible for each. A multi agency approach to information sharing, risk assessment and decision making, that puts the person at the centre and involves the family, is essential in achieving the best possible outcomes for the person.
10.00 The use of control and restraint
10.1 This section reviews practice against local policy and procedure and national guidance on, the prevention and management of violence and aggression, the use of rapid tranquilisation, physical intervention and seclusion.
Prevention and management
10.2 The Mental Health Trust policy [24] states that ‘All service users identified as at risk of violent and/or aggressive behavior will have a comprehensive risk assessment. The service user and their family/carer (if appropriate) will be involved in the risk assessment. The risk assessment should be reviewed at planned/regular intervals or sooner if the service user’s presentation/ behavior changes.’ Neil did not have a risk assessment that outlined how aggressive or violent behavior should be managed. The risk management plan on admission to Hamilton House says that Neil is at risk of violence to others, but nothing follows on the management of this risk.
10.3 Hamilton House has a similar policy [25]. It recommends that de-escalation is used to prevent challenging behavour and that it is based on a knowledge of the person and causes of behavior. Staff were instructed by the care home manager not to add to chaotic thought by giving too much verbal input at once. ‘A gentle but firm and persistent approach of saying his name is more effective at enabling Neil to respond’. This was a positive approach but there is no evidence of further guidance on how to prevent Neil from becoming more agitated and at risk of harming himself.
10.4 Neil did not have a history of aggression and violence to others, apart from his mother. He did have a history of self abuse and suicidal tendencies. The staff at Hamilton House were concerned that Neil would harm himself. His bedroom was in disarray and he had upturned the bed mattress. A member of staff expressed concern that there were springs in the mattress that Neil could use to harm himself. A number of actions could have been taken at this point, had there been a risk assessment and plan. The least restrictive option might have been to make Neil’s environment safe, for example by removing the mattress from his bedroom. At this stage there were two police officers in Neil’s room. A police officer took hold of Neil’s arm and tried to pull him away from the mattress. Events escalated from here as Neil was restrained on the floor by two police officers and handcuffed. The presence of uniformed police officers did little to prevent and de-escalate and is likely to have increased Neil’s anxiety.
10.5 ’When de-escalation and disengagement techniques have failed the policy says that a risk assessment should be carried out before further restrictive physical interventions are used’.
10.6 This again highlights the importance of a well informed, comprehensive assessment and care plan that takes account of the person’s past history, and is sensitive to what might trigger an aggressive incident and what might work best to diffuse the situation and de-escalate. The staff at Hamilton House knew very little about Neil. They were dependent upon the risk assessment completed by a mental health nurse that did not know Neil just prior to his admission and a letter with the outcome of Neil’s last CPA meeting. This review has already noted that neither of these assessments was well informed.
[24] Prevention and management of Violence and Aggression C66, NSFT
[25] Managing behaviours that challenge others policy, 2.12.2013 Prime Life
10.7 The risk assessment prepared prior to Neil’s admission to Hamilton House identified the risks of self harm and aggressive behavior however, there was not a thought through plan on how to reduce the risk of violent or aggressive behavior occurring and de-escalation strategies. As a result of this lack of planning and communication, interventions were reactive and the roles of different professionals unclear. The police were restraining Neil as they had been called to assist, but in hindsight this could have been avoided with better planning and communication.
Rapid tranquilisation
10.8 The National Institute for Clinical Excellence (NICE) says that ‘Rapid tranquilisation should only be used based on clinical need (e.g. where the service user is highly aroused, agitated, overactive, aggressive or making serious threats or gestures towards others or is destructive to their surroundings and is therefore placing their safety or that of others at risk and when other therapeutic interventions have failed to contain the behaviour’.
10.9 Neil was prescribed Lorazepam (a sedative used to treat acute anxiety) and Haliperidol (used to treat agitation, aggression and restlessness) by the CRHT team when they were contacted by Hamilton House who reported that Neil was distressed and had a high level of auditory hallucinations and his speech pattern was described as ‘word salad’. At this time Neil was distressed and agitated but not violent or aggressive. A medical examination was not carried out prior to this prescription being given, neither was Neil seen by a mental health nurse from the CMHT. Neil’s condition deteriorated and he became violent and aggressive towards himself and his surroundings. He did not at any time threaten or harm staff.
10.10 The use of rapid tranquilisation to sedate Neil and keep him safe from self harm may well have been the most appropriate course of action. However, it might have been delayed had preventative interventions by skilled mental health professionals taken place when Neil first became agitated. There is no record of the risks, benefits and alternatives being discussed with Neil or his sister as recommended in the mental health act policy on rapid tranquilisation.[26]
[26] NSFT Rapid Tranquilisation policy C11 version 02
10.11 The mental health trust policy is clear about the physiological observations and monitoring that must be carried out following rapid tranquilisation, this includes:
- The service user must be placed ‘within eyesight observations’
- Temperature, pulse and respiration checked every 15 mins for 4 hours after the injection(s) have been given. Thereafter monitor half hourly until the service user is ambulatory
- Blood pressure 30 mins and 60mins after the injection(s)
10.12 All of the chronology entries for administration of rapid tranquilisation and for observation and monitoring from the 9th January to the 11th January have been collated in table seven – records of observation and monitoring. There are two entries that say observations could not be carried out as Neil was too agitated. Some entries for administration of medication are not followed with an entry on observations. If Neil’s physiological observations were monitored as recommended in the mental health trust’s policy, then this has not been recorded in the chronologies provided.
10.13 Table seven – Records of observation and monitoring
9/1/14 Night Shift record 09/01/2014 to 10/01/2014 PRN Lorazepam 1 mg at 20.50 hrs and again 04.30 after NJ began shouting/banging doors etc.
Prime Life Care plan daily record
10/1/14 He was offered Haloperidol 5 mg PRN which he accepted. A further PRN Lorazepam 1 mg PRN given to try and alleviate NJ’s agitation. Neil’s observations have not been done as he has been non-cooperative with this. Neil awake 04.45 and in bed – allowed staff to check his obs BP 100/54 P98 and temp 36.6.
Prime Life Care plan daily record
1011/1/14
PM (Night 10/01/2014) “Neil nonconcordant with taking of obs” AM 04.55 (11/01/2014) Pulse = 98. Temperature = 36.6
Prime Life Care plan daily record
11/1/14 Medication; 15 mgs (3x 5mgs) Haloperidol given PRN and 6 mgs Lorazepam (4x 1mg, 1x 2mgs) given PRN and 50mgs (1x 50mgs) Promethycine – in 24 hrs*.
NSFT Patient record
11/1/14 Transferred to seclusion room at 19.05pm, PRN Lorazepam at 19.13pm, locked at 19.15pm.
NSFT Patient record
11/1/14 Medical review at 19.30pm; P1 bruising noted to hands and back, agitated, hallucinations. Unable to physically examine due to agitation. Plan; when more settled physically examine, PRN Lorazepam (rapid tranq IM). NSFT Patient record
11/1/14 Medical review by P2 at 21.30pm; remained agitated, attempting to self harm, head banging. Plan; review at 2hrs via phone, continue seclusion, IM Promethazine and Haloperidol (rapid tranq)
NSFT Patient record
1112/1/14 Nursed in seclusion; observed 10 minute intervals, water at 10.05am on 12/01/2014. Physical examination at 10.35am by P1; physical observations within normal limits. 11.40am; further drink of water.
NSFT Patient record
Physical intervention (restraint)
10.14 Both the mental health trust policy and that of Prime Life are clear that physical intervention (restraint) must always be used as a last resort and be reasonable, proportionate and justifiable.
10.15 The Mental Health Act, Section 6 says that, ‘restraint is only permitted if the person using it reasonably believes it is necessary to prevent harm to the person who lacks capacity, and if the restraint used is proportionate to the likelihood and seriousness of the harm’
10.16 The Norfolk constabulary IMR explains the use of police powers to exercise force. ‘In this particular instance there would have been a Common Law power to exercise reasonable force in the execution of (police) duties and a power under Section 3, Criminal Law Act 1967 to use reasonable force to prevent crime (e.g. criminal damage to property, assault etc.)’
10.17 When physical force was used to restrain Neil, two policemen physically restrained Neil, handcuffed him using a rear stack and lay him on his side, this was in response to the threat of criminal damage to property, assault and self harm. The use of Criminal Law in using reasonable force contradicts the Mental Capacity Act of a response that is proportionate to the likelihood and seriousness of the harm.
10.18 When the police were asked by a member of staff at Hamilton House to provide assistance in controlling Neil so that he did not harm himself they were put in a difficult position. Mental health professionals should have taken the lead in helping to calm Neil and keep him safe from self harm. The Department of Health (February 2014) recommend that positive behaviour support is used to minimize the need for restrictive interventions. The police had no knowledge of Neil’s history. They were faced with a situation where a man was in a state of undress, his bedroom was in disarray, he was clearly agitated and not responding to verbal requests by the police or care staff. The action that they took in restraining Neil was in response to this immediate situation. It was not ideal and should have been avoided by mental health professionals de-escalating the situation.
10.19 The Independent Commission on Mental Health and Policing (May 2013) says that ‘Mental health is part of the core business of policing. The role of the police is not a clinical one but mental health issues are common in the population and will be found in suspects, victims and witnesses.’ However, the police should not be managing complex situations on their own, they should be supported by health and social care staff. It is not appropriate to call on the police to manage a situation that should be managed by skilled mental health staff.
10.20 There was an opportunity for mental health professionals to reassess the situation with the police and to plan a more appropriate way of restraining Neil. For Neil to continue to be restrained with Emergency Restraint Belts, handcuffed and lying prone for the duration of his wait and journey to Suffolk, a period of over two hours was unacceptable.
10.21 The situation with Neil escalated as he became more agitated when the police intervened. The Independent Commission on Mental Health and Policing found that many people with poor mental health often became afraid and more aggressive when the police tried to restrain them. Without the knowledge of a person’s history the memories and fears that a police uniform or the act of handcuffing and restraining may arouse are not understood. Once the police had started a process of restraint it may have been difficult for them to step back and mange the situation in a different way. Health and social care professionals allowed the police to determine the level of restraint and force used.
10.22 The policy for police using control and restraint is not dissimilar to that of the mental health trust and the care home. ‘Statute and common law provide that police use of force against an individual must be necessary and reasonable. Restraint must be proportionate to the situation, applied for the minimum time required and used as a last resort as part of a range of various de-escalation strategies. In addition under the Mental Capacity Act the restraint of a person who lacks capacity must be in the person’s best interests’ (Independent Commission on Mental Health and Policing May 2013).
10.23 Two more police officers joined their colleagues. They used Emergency Restraint Belts (ERBs) to control Neil. One was placed around the upper half of his body, the other around his legs. Neil was lifted and placed prone on a portable stretcher to be transported by ambulance to Wedgewood House (West Suffolk). The journey took one hour and twenty minutes. There are a number of risks associated with prolonged application including; neuropraxia, joint dislocation. Skin pressure effects and chest compression. ACPO guidance states that External Restraint Belts (ERB) should be a temporary measure and ideally removed within 30 minutes [27]. Attention should be given to check that the straps are not to tight and regular observations made to asses for any breathing difficulties or pain caused by over tightening of the straps.
10.24 An Inquiry into the death of David Bennett (Norfolk, Suffolk and Cambridgeshire Strategic Health Authority Dec 2003) recommends that, ‘Under no circumstances should any patient be restrained in a prone position for a longer period than three minutes.’
10.25 David Bennett was an African-Caribbean man suffering from schizophrenia who had been involved in an incident with another patient whilst an in-patient at a mental health hospital. When he was moved to another ward he was violent towards a nurse. He was restrained by a number of nurses and placed in a prone position, face down on the floor. During the prolonged struggle that continued he collapsed and died.
10.26 Dr Cary, a Consultant Forensic Pathologist who carried out a post mortem on David Bennett at the request of the Bennett family said: “Prone restraint is an area that we know from cases around the world is a position in which people appear to die suddenly when they are restrained for long periods. And that I think is a matter of fact. There is some debate however, as regards what sort of mechanisms may be involved in causing those deaths. But we do know that the deaths occur, firstly when people have been restrained in the prone position in particular. And just to clarify that, that means that they are face downwards, lying down. And secondly, that the deaths seem to occur when the restraint and the struggling against the restraint goes on for a long period and those, as I say, are two quite well established facts.’ (Inquiry into the death of David Bennett Dec 2003).
10.27 A statement by one of the paramedics in attendance [28] says ‘The patient was placed on his right hand side in order to keep his airway clear although he kept turning his head down into the stretcher.’ He goes on to say, ‘He continued to turn his face into the stretcher and his body was slightly over to the right hand side so I placed a rolled up blanket under his head to give him more support and keep him a bit more upright to prevent him pushing his head into the stretcher.’ It is possible that Neil was not in a prone position for the duration of the journey. However, CCTV film shows clearly that Neil was strapped in a prone position to the stretcher when he arrived at Wedgewood House.
10.28 The handcuffs that held Neil’s hands behind his back in a ‘rear stack’ position from the time he was restrained at Hamilton House until he arrived at Wedgewood House left lacerations on his wrists [29]. These cuts and bruises to his left shoulder and back are recorded on a body map in his care plan [30].
[27] ACPO Personal Safety Manual Module 04 Medical Implications. 28 Operation Madeley statement S41
10.29 When Neil was transferred to a Psychiatric Intensive Care Unit Bed a private secure ambulance was used. This ambulance had a secure cell so that Neil could be observed and was safe from harm without the need for any physical restraint. The private ambulance service use soft handcuffs when there is the need to physically restrain someone. In hindsight the secure private ambulance would have been better suited to Neil’s needs when he was transported from Hamilton House to Wedgewood House. The Approved Mental Health Practitioner (AMHP) who arranged Neil’s transport was aware of this service but understood that the NHS ambulance should always be the first choice for NSFT patients and secondly that it would take some time for the secure private ambulance to travel to Norfolk as it is based outside of the county.
10.30 The Approved Mental Health Practitioner (AMHP) has professional responsibility for all the necessary arrangements to be made for the conveyance of the person to hospital. They must ensure that they are conveyed lawfully, humanely and should give guidance on their care (Mental Health Act [31])
Seclusion 10.31 ‘Seclusion is the supervised confinement of a patient in a room, which may be locked to protect others from significant harm. Its sole aim is to contain severely disturbed behavior, which is likely to cause harm to others.’ Mental Health Act [32].
10.32 Neil was secluded at 10.45 on the 11th January. He had been placed in the Section 136 suite [33] because the low stimulus area within the ward was already in use. ‘Neil was consistently leaving the room and banging doors, he had undressed and the decision was made to seclude him due to his dignity and vulnerability.’ [34] The reason for seclusion recorded on the seclusion record and observation charts is ‘Highly agitated, incoherent and distressed, markedly paranoid in affect’. [35]
10.33 The reason for secluding Neil has to be questioned. The sole aim of seclusion is to contain severely disturbed behavior, which is likely to cause others harm. The reasons given for secluding Neil do not refer to the risk that he might harm others. From the start of this very disturbed episode Neil has been reported as being verbally aggressive, violent towards himself and damaging property. There have been no reports of violence towards others or threats that he will harm others.
[29] Operation Madeley photograph of copies of injuries wxhibit SG/1
[30] Operation Madeley Manual handling and assessment plan D45
[31] Mental Health Act code of practice (2008) 15.17-15.30
[32] Mental Health Act code of practice (2008) 15.4
[33] 136 suite is an environment used for patients detained under section 136. That is when a police officer believes a person needs a place of safety until they can be properly assessed.
[34] NSFT IMR
[35] Operation Madeley D16
10.34 The mental health trust policy states that ‘seclusion should be used as little as possible and for the shortest period of time. It is not to be used because of staff shortages or because the environment is being damaged, unless the welfare of others is compromised’. [36] Neil was in seclusion from 10.45 on the 11th January to 18.00 when he was transferred by ambulance to the PICU. Here he was secluded from 19.05 on the 11th January to 16.35 on the 12th January when he was observed to have stopped moving, just over 28 hours.
10.35 During this period of seclusion Neil had regular fifteen minute checks. This was in line with the mental health trust policy at the time. Since then the trust policy has changed to five minute checks.
10.36 The mental health trust policy also states that ‘all physical needs of patients, toilet, food and drink and personal hygiene must be met while the patient is secluded. It is noted in the mental health trust IMR that, ‘there is no evidence of Neil having drunk water, or received any nutrition between the hours of 09.00 on the 11th January and 10.05 on the 12th January, a period of over 24 hours. This is being taken very seriously by the mental health trust and acted upon.
10.37 Attending to Neil’s physical health needs whist in seclusion is addressed further in the next section.
10.38 Neil experienced physical restraint, rapid tranquilisation and seclusion in a period of 48 hours. He was clearly displaying severely disturbed behavior and staff managed the best that they could. However, a well informed risk assessment and plan that addressed how professionals and agencies could work together to minimize risk and act in Neil’s best interests may have prevented the situation escalating and staff feeling out of control.
10.39 When Neil presented himself at the Clozapine Clinic to ask for help he was recorded as being ‘entirely amenable to whatever intervention was suggested’ [37] A more informed risk assessment might have anticipated the need to protect Neil from harming himself. It might have been possible to discuss his needs and wishes with him at this time including the preparation of an Advance Statement [38]. Neil’s sister might also have been involved so that she could discuss the risks with Neil and share her own views.
[36] NSFT Seclusion and Long Term Segregation C107 Version 04
[37] NSFT risk assessment 6/1/2014
[38] A written record of how a person would like to be treated if they lose the capacity to make decisions about their care.
11.0 Attention to physical health needs.
11.1 This section addresses how the physical health needs of Neil were met during his hospital stay in January and how primary and secondary care services worked together to monitor Neil’s physical health needs.
11.2 The Department of Health (February 2014) stresses the importance of integrating physical and mental health care. People with schizophrenia tend to have poor physical health and a shorter life expectancy as a result of an unhealthy lifestyle- poor diet, lack of exercise, smoking, low income, lack of employment and social isolation.39 The Department of Health recommends annual health checks and strengthening the role of the GP in working with mental health professionals to provide integrated health and social care.
11.3 When Neil presented himself at the Clozapine clinic to seek help the care coordinator carried out an assessment of his mental health needs. This did not include a physical health assessment. The GP could have made a valuable contribution to this assessment.
11.4 South Norfolk CCG requires all patients admitted to a mental health hospital to have a physical health check on admission. This is so that physical health symptoms are not overshadowed by a focus on mental health. This requirement does not apply to other providers and so when Neil was admitted to Hamilton House a physical health check was not carried out. Whether or not this would have identified an underlying physical health problem is unknown. However, it would be good practice to include this requirement for all mental health providers.
11.5 When Neil was admitted to Wedgewood House he had been reintroduced to Clozapine after a short period of non-compliance, he had also been taking Lorazepam (a benzodiazepine), he had been restrained in the prone position and he had been banging his head hard against the wall. All of these presented risks to his physical health and so health checks at regular intervals and close monitoring of his physical condition was essential.
11.6 Neil’s re-titration plan was for increasing doses of clozapine to be administered each day until the previous prescription level was reached. Table eight below shows the prescribed and administered medication for Neil’s re-titration plan.
[39] http://www.rethink.org (accessed 24/6/2015)
11.4 Table eight Re-titration plan
Day one 07/01/2014 12.5mg Administered
Day two 08/01/2014 25mg Administered
Day three 09/01/2014 50mg Administered
Day four 10/01/2014 75mg Administered
Day five 11/01/2014 100mg No record
Day six 12/01/2014 125mg No record
Day seven 13/01/2014 150mg No record
11.7 Neil’s inpatient management plan dated 11th January says that Neil was previously taking 350mg of Clozapine before missing several doses. The plan says for Clozapine to ‘recommence on 13th January following a review by the ward consultant’. A statement by an expert advisor for Operation Madeley says, ‘I have seen no evidence that Clozapine was administered to Neil after the 10th January. [40]
11.8 Treatment with Clozapine has to start carefully because the first few doses can cause the blood pressure to fall, especially on standing, a condition called orthostatic hypotension. Benzodiazepines, might increase the risk of severe orthostatic hypertension with Clozapine. Sudden withdrawal of Clozapine can lead to rebound psychosis and other withdrawal symptoms [41]
11.9 Between the 10th and 12th January Neil was administered tranquilisers in the form of Lorazepam (a benzodiazepine) and Haloperidol. Given the risks to Neil’s physical and mental health of both, a sudden withdrawal from Clozapine and the combination of Clozapine and a benzodiazepine he should have been closely monitored with frequent and regular health checks.
11.10 The mental health trust policy on physical restraint says that, ‘physical intervention in any position has risks including positional (postural) asphyxiation, cardiac arrest/respiratory distress’. It goes on to say that ‘Service users who have been restrained in a prone or supine position should be reviewed immediately by a member of medical staff’. This is a requirement of the Mental Health Act (2008) code of practice.
11.11 The mental health trust policy on rapid tranquilisation says that following the use of rapid tranquilisation an ECG should be carried out at the earliest opportunity.
11.12 Neil’s inpatient management plan did not address the increased risk to Neil’s physical and mental health as a result of the factors described above. The plan had a section on monitoring physical health needs, these were routine checks and did not include an ECG.
[40] Operation Madeley Statement Physician Clinical Pharmacologist and Director S49 41 From statement S49 (as above)
11.13 Neil had medical reviews on the 11th and 12th January (see table seven). The first of these at 19.30 on the 11th January says, ‘unable to physically examine due to agitation’. The next medical review at 21.30 says that Neil is still agitated. It is not until the next day 12th January that Neil has a physical examination at 10.35. The mental health trust IMR says that ‘a medic advised physical examination and ECG on the 11th January but this did not proceed. The physical examination on the 12th January did not include an ECG.’
11.14 Neil may have been too distressed and agitated for staff to carry out the observations and health checks that the mental health trust policy requires. However, the risk management plan and care plan do not acknowledge the increased risks to Neil’s health as a result of his medication, physical restraint, rapid tranquilisation and head banging. There is no record to show what actions were taken to address this challenge apart from not carrying out the checks.
11.15 People with schizophrenia have an increased risk of death from coronary heart disease (HQIP & RCP 2012). Monitoring of cardiometabolic risk factors should be routinely carried out by secondary or primary care (NICE 2014) however how this responsibility is divided between primary and secondary care is not specified in NICE guidance. There is a recommendation GPs and primary healthcare professionals monitor the physical health of people with psychosis or schizophrenia when responsibility for monitoring is transferred from secondary care and then at least annually.
11.16 The following risk factors should be monitored:
- Body mass index
- Blood levels of glucose, lipids (total cholesterol and HDL)
- Blood pressure
- Use of tobacco
- Excessive use of alcohol
- Substance misuse
- Prolactin (if indicated)
- History of cardiovascular disease in the person’s family.
11.17 GP records show that Neil’s body mass index, cholesterol, HDLC, Urea and electrolytes, liver function tests, plasma glucose tests and blood pressure were routinely carried out. This monitoring is in response to the Quality Outcome Framework (QOF) requirement of GP’s for keeping a register on the health checks carried out on adults with schizophrenia.
11.18 A letter from Neil’s psychiatrist to his GP dated the 12th July 2013 says that Neil has been discharged from CPA and asks the GP to continue to monitor his physical health annually.
11.19 Neil was asked about his use of tobacco, alcohol and other substances he might abuse at his medical reviews. He did admit to drinking three pints of lager a day at his last CPA review but the GP found that his liver test to be relatively normal. Neil’s sister did not think that he had abused alcohol or drugs and it so it was not considered to be a risk.
11.20 Monitoring of cardiometabolic risk factors by primary and secondary care seems reasonable as it covers the requirements of NICE guidance. However, it has not been done in a purposeful way with agreement between primary and secondary care on how they work together. The results of the monitoring of cardiometabolic risk factors did not give any cause for concern.
12.0 Conclusion
12.1 Neil struggled to live independently with paranoid schizophrenia and for several years managed this quite successfully with the support of care coordinators who knew him well and CPA. When the mental health trust went through a reorganization as part of a cost improvement strategy, the level of support Neil received reduced significantly. When Neil reached a crisis point in January 2014 he did not have the infrastructure of care and support that had successfully helped him to manage similar crisis in the past. Neil ran out of medication and although it is not entirely clear how this happened it is evident from records that sufficient Clozapine was prescribed. Neil had been non-compliant with medication in the past; this is one of the manifestations of his self neglect.
12.2 When Neil presented himself at the Clozapine clinic to seek help, the opportunity to carry out a well informed comprehensive assessment and risk management plan with Neil and his family was missed. The lack of multi agency information sharing, comprehensive informed assessment and risk management planning is a recurring theme in this review of Neil’s care.
12.3 The use of physical control to restrain and the use of seclusion did not meet with national and local policy or in some instances with the requirements of the Mental Health Act. A well informed assessment and risk management plan that was understood and owned by all of the agencies involved in Neil’s care could have reduced the potential for reactive, disproportionate responses and a confusion over the roles of different agencies and teams.
12.4 The NHS should take responsibility for people in mental health crisis and provide responsive and timely services. The police should be supported by health professionals in managing people in mental health crisis and should only be asked to assist in managing patient behavior in exceptional circumstances (Mental Health Crisis Care Concordat).
12.5 Decisions were made about Neil’s care based on the availability of appropriate in patient hospital beds. The lack of suitable beds in Norfolk resulted in Neil’s admission to a care home and then to an inpatient bed in the neighbouring county of Suffolk before being transferred to a specialist PICU bed. Health and Social Care Partnerships in Norfolk and Suffolk have signed up to the Mental Health Crisis Concordat [42] which makes a commitment to ensure adequate mental health services are provided to support people before a crisis point is reached and urgent and emergency access to crisis care. If the action plans of the local concordat are to make a real difference to the lives of people like Neil then they need to be considered against the findings of this review.
13.0 Recommendations
13.1 SAB to ensure that partners work together with adults who self-neglect to minimize the risk of harm and respond in a timely and proportionate way if the risk escalates.
13.2 SABs to be assured that all partners raise the awareness and understanding of staff who work with people that self-neglect , so that flexible, personcentred and creative approaches are encouraged and supported to nurture self-care.
13.3 SAB and partners to work with citizens, local businesses and community facilities to raise the awareness of safeguarding adults, particularly hate crime and financial abuse and engender a shared responsibility for prevention within the community.
13.4 SAB and partners to take specific steps to strengthen the important role of family and loved ones and where appropriate involve them in planning a person’s care, recognizing that when a person has mental capacity that they have the right to make what might be considered unwise decisions.
13.5 Senior leaders and their organisations when considering proposals for organizational change or reduction of services, take into account the impacts on safeguarding and in the spirit of openness and transparency share concerns with the partnership so that a partnership approach can be taken to minimizing potential risks.
13.6 SABs to Agree a joint approach to the assessment and management of risk to vulnerable adults across agencies that identifies the circumstances in which there is the need for a structured partnership approach, clarifies the roles of agencies and professionals and identifies a lead professional. This may be through use of the CPA, or by other agreed means if CPA is not appropriate.
13.7 SABs to ensure mechanisms are built in to assure the quality of care assessment and decision making across partner agencies. In line with national guidance, when a decision is made to discharge someone from CPA there should be:
- An appropriate review and handover (eg to the lead professional of GP)
- An exchange of appropriate information with all concerned, including carers
- Plans for review, support and follow up, as appropriate
- A clear statement about the action to take, and who to contact, in the event of relapse or change with a potential negative impact on that person’s well-being.
[42] http://www.crisiscareconcordat.org.uk/areas/suffolk/ http://www.crisiscareconcordat.org.uk/areas/norfolk/
13.8 SABs to challenge, improve and promote a shared agreement and mechanisms (eg health passport) to ensure improved communication and information sharing within and across agencies so that information is accurate, timely and well informed, to ensure a person’s safety and wellbeing. This to specifically include that a person’s relevant history follows them through their passage of care so that each professional or clinician has the correct information to make informed decisions critical to their wellbeing.
13.9 SABs to consider how information and intelligence that in its own right may not be cause for concern is brought together so that cumulative risk can be identified and acted on, to safeguard vulnerable adults.
13.10 SAB partners to share information as appropriate, about the ways in which people in mental health crisis are provided with appropriate support and treatment and to benchmark services against the standards published in the Mental Health Crisis Concordat.
13.11 All SAB partner agencies to ensure that the use of all types of restraint for people with mental health conditions in any setting, is safe, proportionate and necessary, with policy being appropriate and implemented effectively, and use of restraint monitored.
13.12 SABs and the partner organisations to take robust action to eliminate the use of restraint in the prone position, in line with overarching professional or regulatory guidance, and to regularly review data on use of prone restraint.
13.13 SABs to improve knowledge of and appropriate access to specialist ambulance transportation for patients with challenging behaviour that are at risk of harming themselves or others; to review the patient conveyance procedure and to lobby for access to secure ambulance transportation when it is needed.
13.14 SABs to agree a joint protocol between the police, mental health trust, local authorities and CCG on the role of each agency and profession in managing challenging behaviours of vulnerable adults, where restraint or control is being considered.
References
Local Government Ombudsman and Parliamentary and Health Service Ombudsman, Investigation into a complaint against South Essex Partnership Trust and Bedford Borough Council, Ref JW 111510 and 11010604 May 2014
Suzy Braye, David Orr and Michael Preston-Shoot, Self-neglect policy and practice: key research messages, March 2015, SCIE London
Department of Health Refocusing the Care programme Approach: Policy and positive practice guidance, March 2008, London
National Institute for Clinical Excellence, Service user experience in adult mental health: improving the experience of care for people using adult mental health services, (NICE guidance CG136) December 2011, London http://www.nice.org.uk/guidance/CG136/chapter/1-Guidance accessed 30/04/15
National Institute for Clinical Excellence, Psychosis and schizophrenia in adults: treatment and management, (NICE guidance CG178) February 2014, London
Department of Health Refocusing the Care Programme Approach: Policy and Positive Practice Guidance, March 2008 London
SCIE Guide 53 Adult Safeguarding for Housing Staff, April 2014 http://www.scie.org.uk/publications/guides/guide53/ accessed 4th May 2015
Independent Commission on Mental Health and Policing Report, May 2014, Mental Health and Policing Commission, Metropolitan Police, London http://news.bbc.co.uk/1/shared/bsp/hi/pdfs/10_05_13_report.pdf accessed 7th May 2014
An Inquiry into the death of David Bennett, December 2013 Norfolk, Suffolk and Cambridgeshire Strategic Health Authority An inquiry under HSG(94)27
Report of the National Audit of Schizophrenia (NAS) 2012, Health Quality Improvement Partnership (HQIP) and Royal College of Psychiatrists, 2012, London
Appendix One
Documents reviewed from Operation Madeley
D12 Copy form A3 dated 11/01/14 Joint recommendation for admission for assessment completed by Dr k and Dr P.
D14 Copy daily record of events re care at HH D15 Copy of Clinnote print out – details of accompanied journey to HH and that Neil states confused with clozapine so did not take it, plan to re-titrate
D16 Copy risk profile 11/01/14 L ward
D17 Risk profile L ward
D18 Copy for H3 record of detention in hospital L ward
D19 Copy EPEX notes print out – how he arrived at S ward and phone calls made to L ward
D20 Admission form to L ward from S ward
D25 Copy nursing log L ward
D26 Seclusion record/observation chart L ward
D27 Copy risk profile, L ward
D28 Photos of injuries to Neil
D30 Letter to GP from Psychiatrist outcome from CPA review resulting in discharge from CPA
D36 Copy observation form completed whilst in ICU
D37 Copy inpatient management plans L ward
D42 Copy of form authorizing transfer to WH under S2 MHA
D45 Copy of Admissions checklist SWard
D46 Copy of form A2 Application for admission for assessment
D47 Copy papers re the transfer of Neil from S ward to L ward
D48 Copy of ambulance service care record re transport of Neil to WH
D59 Copy HH pharmacy doc
D111 Rapid tranquilisation policy, NSFT
D119 Seclusion and long term segregation policy V3 NSFT
D120 Seclusion and long term segregation policy V4 NSFT
D121 Transfer between clinical teams within the trust NSFT
D122 Physical intervention (restraint) policy V2 NSFT
D123 Transfer to and from acute hospital (planned and emergency) V3 NSFT
D124 Prevention and management of violence and aggression V3 NSFT
D127 AMHP report
D135 Copy of photographs showing conditions of cleanliness of Neil’s flat
D149 Email from Dr K stating he does not carry medication when conducting MHA assessments and does not sedate pts as he has to be able to assess the patient.
D158 Copy clozapine distribution log book includes an entry showing one months supply to cover 02/12-13/01/14
D159 Copy medication history showing 8 weeks supply dispensed on 27/11/13
D163 Emails 19/9/14 from Prof Ferner addressing queries raised regarding medication
R9 Expert report statement relating to the use of restraint used
S25a Statement Pharmacy technician
S33 Statement last Care Co-ordinator
S37 Statement AMHP
S41 Statemnt EofE Ambulance staff
S49 Expert report on medication dispensed and its likely effect of
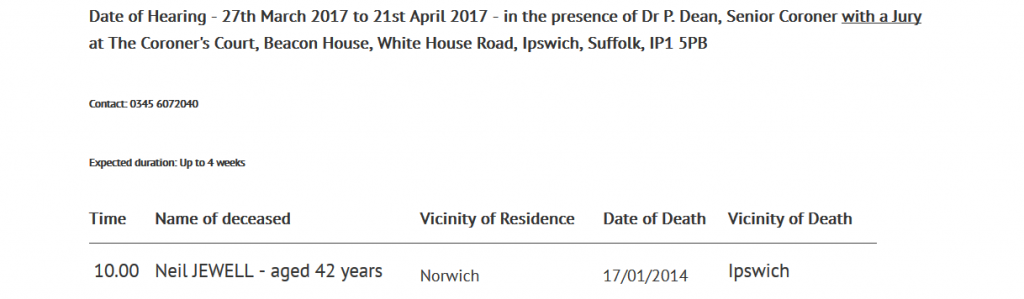


Your article helped me a lot, is there any more related content? Thanks! https://accounts.binance.com/bg/register-person?ref=WTOZ531Y
I was able to find good info from your blog articles.
My web blog; vpn coupon code 2024
After checking out a number of the blog articles on your web
page, I honestly appreciate your way of blogging.
I book marked it to my bookmark site list and will be checking back in the near future.
Please check out my website as well and tell me how you feel.
Feel free to surf to my blog post vpn special code
reputable indian pharmacies http://indiaph24.store/# buy medicines online in india
pharmacy website india
medication from mexico pharmacy: mexico pharmacy – buying from online mexican pharmacy
mexican drugstore online: Online Pharmacies in Mexico – mexican pharmacy
india online pharmacy Cheapest online pharmacy indian pharmacies safe
http://mexicoph24.life/# pharmacies in mexico that ship to usa
mail order pharmacy india indian pharmacy ?»?legitimate online pharmacies india
https://nolvadex.life/# buy tamoxifen
lisinopril 30 mg price: lisinopril 20 mg canadian pharmacy – lisinopril 10 mg price
https://lisinopril.network/# lisinopril sale
buy ciprofloxacin over the counter ciprofloxacin generic price cipro online no prescription in the usa
ciprofloxacin 500 mg tablet price: buy ciprofloxacin – ciprofloxacin over the counter
http://cytotec.club/# cytotec pills buy online
http://ciprofloxacin.tech/# ciprofloxacin order online
buying generic propecia price: order cheap propecia – buying cheap propecia no prescription
get generic propecia buying generic propecia without dr prescription buy cheap propecia
https://finasteride.store/# order propecia without prescription
cytotec pills buy online: buy cytotec online – purchase cytotec
https://lisinopril.network/# 40 mg lisinopril for sale
https://finasteride.store/# get propecia online
liquid tamoxifen tamoxifen mechanism of action liquid tamoxifen
buy cytotec over the counter: cytotec pills buy online – purchase cytotec
https://nolvadex.life/# nolvadex pct
how c?‘n i get cheap propecia pills get propecia cost propecia tablets
cipro online no prescription in the usa: buy generic ciprofloxacin – ciprofloxacin generic
https://finasteride.store/# propecia online
https://finasteride.store/# order cheap propecia tablets
ciprofloxacin: where can i buy cipro online – cipro for sale
http://cytotec.club/# cytotec abortion pill
cheap propecia without prescription: buying cheap propecia without rx – get propecia online
what is tamoxifen used for nolvadex for sale tamoxifen breast cancer
http://finasteride.store/# propecia without rx
buy cipro online: cipro – antibiotics cipro
cheap propecia tablets cost generic propecia tablets order generic propecia without rx
http://finasteride.store/# cost cheap propecia pill
nolvadex for sale amazon tamoxifen blood clots does tamoxifen cause bone loss
buy cytotec online fast delivery: buy cytotec over the counter – buy cytotec pills
http://lisinopril.network/# lisinopril 12.5 mg price
purchase cipro where can i buy cipro online cipro for sale
https://lisinopril.network/# lisinopril tabs 20mg
tamoxifen postmenopausal: tamoxifen moa – tamoxifen effectiveness
https://viagras.online/# Generic Viagra for sale
Buy Tadalafil 20mg buy cialis overseas buy cialis pill
http://viagras.online/# cheap viagra
Kamagra 100mg price kamagra.win Kamagra 100mg
Kamagra 100mg price: buy kamagra online – super kamagra
https://cenforce.pro/# buy cenforce
buy cialis pill Generic Tadalafil 20mg price cheapest cialis
http://viagras.online/# Sildenafil Citrate Tablets 100mg
https://cenforce.pro/# Cenforce 150 mg online
Levitra 20 mg for sale buy Levitra over the counter Generic Levitra 20mg
https://viagras.online/# viagra canada
http://viagras.online/# Viagra Tablet price
viagra canada: Buy Viagra online cheap – Generic Viagra for sale
Kamagra 100mg kamagra.win cheap kamagra
http://kamagra.win/# ?»?kamagra
Levitra online pharmacy Cheap Levitra online Buy Vardenafil 20mg online
https://pharmcanada.shop/# canadian pharmacy service
buy pills without prescription how to get prescription drugs from canada canadian and international prescription service
https://pharmworld.store/# online pharmacy no prescription
online canadian pharmacy coupon: online pharmacy – rx pharmacy no prescription
https://pharmcanada.shop/# canadian online pharmacy reviews
us pharmacy no prescription canadian pharmacy coupon pharmacy coupons
is canadian pharmacy legit: canadapharmacyonline legit – canadian pharmacy 24h com
mexican pharmaceuticals online: purple pharmacy mexico price list – mexico drug stores pharmacies
http://pharmmexico.online/# mexico drug stores pharmacies
canada drugs online: reliable canadian online pharmacy – cross border pharmacy canada
canadian prescription prices no prescription medication canadian pharmacy without prescription
https://pharmmexico.online/# mexican mail order pharmacies
online pharmacy no prescription: pharm world – cheapest pharmacy to fill prescriptions without insurance
purple pharmacy mexico price list: medicine in mexico pharmacies – buying from online mexican pharmacy
how to order prescription drugs from canada best online pharmacies without prescription buying prescription drugs online canada
https://pharmworld.store/# online pharmacy no prescription needed
medicine in mexico pharmacies: best online pharmacies in mexico – mexican drugstore online
mexico drug stores pharmacies buying prescription drugs in mexico buying from online mexican pharmacy
http://pharmcanada.shop/# pharmacy in canada
generic doxycycline buy doxycycline hyclate 100mg without a rx order doxycycline 100mg without prescription
https://prednisoned.online/# prednisone 50 mg for sale
neurontin 300mg: neurontin tablets no script – neurontin 300 mg pill
amoxicillin 500 mg without a prescription amoxil pharmacy 875 mg amoxicillin cost
doxycycline hyclate: generic doxycycline – vibramycin 100 mg
https://amoxila.pro/# where to buy amoxicillin pharmacy
neurontin singapore: cost of brand name neurontin – neurontin 3
buying amoxicillin in mexico: amoxicillin 500mg prescription – amoxicillin 500 mg brand name
how to order doxycycline: buy doxycycline hyclate 100mg without a rx – doxycycline medication
zithromax coupon: zithromax 600 mg tablets – zithromax over the counter canada
neurontin singapore: brand neurontin 100 mg canada – neurontin generic south africa
where to buy amoxicillin: amoxicillin medicine over the counter – how to get amoxicillin
http://amoxila.pro/# amoxicillin cephalexin
zithromax buy online: zithromax over the counter canada – zithromax over the counter canada
http://gabapentinneurontin.pro/# generic neurontin pill
prednisone pharmacy prednisone 40 mg daily prednisone pills cost
zithromax 500 mg lowest price pharmacy online: zithromax tablets for sale – zithromax cost uk
doxycycline generic: generic doxycycline – doxylin
https://prednisoned.online/# 50 mg prednisone canada pharmacy
neurontin tablets: neurontin tablets 300 mg – neurontin prescription medication
zithromax canadian pharmacy: zithromax over the counter – can you buy zithromax over the counter in canada
http://gabapentinneurontin.pro/# neurontin capsules 300mg
zithromax 500 zithromax cost uk generic zithromax online paypal
neurontin generic: purchase neurontin canada – neurontin 300 mg cost
https://gabapentinneurontin.pro/# neurontin online
doxycycline without a prescription 100mg doxycycline online doxycycline
zithromax 500 mg: how to get zithromax over the counter – zithromax 250mg
order amoxicillin online uk: amoxicillin cephalexin – amoxicillin buy canada
http://doxycyclinea.online/# 200 mg doxycycline
54 prednisone: order prednisone 10 mg tablet – prednisone cost in india
purchase prednisone prednisone 4 mg daily can you buy prednisone over the counter
prednisone 20mg cheap: can you buy prednisone over the counter in usa – 20 mg of prednisone
https://zithromaxa.store/# zithromax 250 mg
order amoxicillin 500mg amoxicillin for sale amoxicillin 875 125 mg tab
order amoxicillin no prescription: generic amoxil 500 mg – rexall pharmacy amoxicillin 500mg
where to buy amoxicillin 500mg: amoxicillin 250 mg – amoxicillin capsules 250mg
https://doxycyclinea.online/# buy doxycycline online 270 tabs
amoxicillin 500 mg for sale: generic amoxicillin cost – amoxicillin capsule 500mg price
zithromax coupon: buy zithromax online cheap – cost of generic zithromax
https://doxycyclinea.online/# buy doxycycline cheap
zithromax 250 zithromax over the counter uk buy azithromycin zithromax
neurontin 900 mg: neurontin 100mg discount – medicine neurontin 300 mg
http://zithromaxa.store/# zithromax for sale 500 mg
prednisone buy canada prednisone brand name prednisone tabs 20 mg
buy doxycycline online 270 tabs: buy doxycycline without prescription – doxycycline 100mg
buy doxycycline 100mg: buy doxycycline online uk – buy doxycycline
http://amoxila.pro/# where can i buy amoxicillin without prec
can you buy zithromax over the counter in mexico: purchase zithromax z-pak – zithromax cost australia
zithromax 500 mg lowest price online can you buy zithromax over the counter in mexico zithromax online paypal
amoxicillin 250 mg capsule: buy cheap amoxicillin – can i purchase amoxicillin online
can i buy prednisone from canada without a script prednisone prescription online prednisone ordering online
https://zithromaxa.store/# zithromax 500
buy prednisone online fast shipping: prednisone 10 – prednisone tablets canada
zithromax 250mg: zithromax price south africa – generic zithromax india
prednisone 20mg prescription cost how can i get prednisone prednisone otc price
https://gabapentinneurontin.pro/# neurontin 600 mg price
generic zithromax 500mg india: buy azithromycin zithromax – zithromax online usa no prescription
http://mexicanpharmacy1st.com/# reputable mexican pharmacies online
buying from online mexican pharmacy: mexico pharmacy – buying prescription drugs in mexico online
https://mexicanpharmacy1st.online/# mexican pharmaceuticals online
buying from online mexican pharmacy: buying prescription drugs in mexico online – mexican online pharmacies prescription drugs
http://mexicanpharmacy1st.com/# purple pharmacy mexico price list
mexico drug stores pharmacies: medication from mexico pharmacy – mexican pharmaceuticals online
https://mexicanpharmacy1st.shop/# mexican pharmaceuticals online
pharmacies in mexico that ship to usa: best mexican online pharmacies – mexican online pharmacies prescription drugs
mexican pharmaceuticals online: buying prescription drugs in mexico – mexico drug stores pharmacies
https://mexicanpharmacy1st.com/# mexico drug stores pharmacies
mexican online pharmacies prescription drugs: best online pharmacies in mexico – mexican drugstore online
https://mexicanpharmacy1st.com/# mexican border pharmacies shipping to usa
https://mexicanpharmacy1st.com/# mexican drugstore online
mexico drug stores pharmacies: mexican pharmaceuticals online – mexican border pharmacies shipping to usa
medication from mexico pharmacy: purple pharmacy mexico price list – buying prescription drugs in mexico online
https://mexicanpharmacy1st.com/# buying prescription drugs in mexico
mexico drug stores pharmacies: mexican mail order pharmacies – mexico pharmacies prescription drugs
mexican mail order pharmacies mexican pharmacy mexican rx online
https://mexicanpharmacy1st.online/# mexican online pharmacies prescription drugs
pharmacies in mexico that ship to usa: best mexican online pharmacies – buying prescription drugs in mexico online
mexico drug stores pharmacies mexico pharmacy ?»?best mexican online pharmacies
https://mexicanpharmacy1st.com/# ?»?best mexican online pharmacies
purple pharmacy mexico price list: buying prescription drugs in mexico online – mexico drug stores pharmacies
https://mexicanpharmacy1st.com/# buying prescription drugs in mexico
best online pharmacies in mexico: purple pharmacy mexico price list – medicine in mexico pharmacies
buying from online mexican pharmacy: mexican pharmaceuticals online – mexico pharmacy
https://mexicanpharmacy1st.online/# reputable mexican pharmacies online
reputable mexican pharmacies online: mexico drug stores pharmacies – buying prescription drugs in mexico
get propecia without a prescription: get generic propecia pill – get cheap propecia
buy cytotec over the counter buy cytotec over the counter cytotec buy online usa
https://propeciaf.online/# buy propecia pill
lisinopril 2.5 tablet: lisinopril for sale online – lisinopril 20 mg sale
buying generic propecia pills cheap propecia no prescription cost of propecia
cost cheap clomid: can you buy cheap clomid without rx – cost of generic clomid price
neurontin capsules: cost of neurontin 600mg – cost of neurontin
neurontin cap 300mg price neurontin 400 mg capsules neurontin 50 mg
gabapentin medication: neurontin online usa – neurontin generic cost
https://clomiphene.shop/# can you buy generic clomid no prescription
can i order generic clomid price: where to buy clomid without dr prescription – can i purchase clomid tablets
lisinopril 5 mg canada price of lisinopril 5mg lisinopril 5mg cost
neurontin capsule 400 mg: buy generic neurontin online – neurontin 100 mg capsule
neurontin cost uk neurontin discount neurontin brand name in india
buy cytotec over the counter: ?»?cytotec pills online – buy misoprostol over the counter
http://cytotec.xyz/# cytotec online
generic propecia for sale: get generic propecia – get generic propecia without insurance
order generic propecia without insurance cost of generic propecia price order cheap propecia without a prescription
lisinopril tab 5 mg price: cost of lisinopril 2.5 mg – prinivil cost
get generic propecia prices buying propecia online buying propecia without prescription
where to get clomid pills where to buy generic clomid for sale how to buy generic clomid no prescription
http://lisinopril.club/# lisinopril 30 mg price
https://cheapestindia.com/# reputable indian online pharmacy
best canadian online pharmacy cheapestcanada.com canadian world pharmacy
http://cheapestandfast.com/# mexican pharmacy no prescription
https://cheapestandfast.com/# canadian pharmacy without prescription
buy medication online no prescription cheapest & fast pharmacy best online pharmacies without prescription
http://36and6health.com/# online canadian pharmacy coupon
https://cheapestmexico.shop/# mexican pharmaceuticals online
https://cheapestmexico.com/# medication from mexico pharmacy
india pharmacy reputable indian pharmacies mail order pharmacy india
http://cheapestmexico.com/# mexican online pharmacies prescription drugs
https://36and6health.shop/# cheapest pharmacy for prescriptions
comprare farmaci online con ricetta farmacie online autorizzate elenco acquisto farmaci con ricetta
vente de m̩dicament en ligne: pharmacie en ligne Рpharmacie en ligne pas cher
online apotheke: medikament ohne rezept notfall – online apotheke versandkostenfrei
vente de m?©dicament en ligne ?»?pharmacie en ligne france pharmacie en ligne pas cher
farmacias direct: farmacia online barcelona – farmacias online seguras
online apotheke g??nstig: europa apotheke – g??nstigste online apotheke
http://eumedicamentenligne.com/# pharmacie en ligne
online apotheke versandkostenfrei g??nstigste online apotheke g??nstige online apotheke
farmacie online sicure: acquisto farmaci con ricetta – migliori farmacie online 2024
farmacias online seguras en espa?±a farmacia online espa?±a env?o internacional farmacia barata
medikamente rezeptfrei: medikamente rezeptfrei – beste online-apotheke ohne rezept
farmacia online 24 horas: farmacia online 24 horas – farmacia online env?o gratis
Farmacia online più conveniente: acquistare farmaci senza ricetta – farmaci senza ricetta elenco
?»?Farmacia online migliore: farmacia online pi?? conveniente – Farmacia online miglior prezzo
apotheke online internet apotheke europa apotheke
https://eufarmacieonline.shop/# migliori farmacie online 2024
Farmacia online più conveniente: Farmacia online più conveniente – Farmacie on line spedizione gratuita
farmacia online madrid: farmacia online madrid – farmacia online env?o gratis
ohne rezept apotheke online apotheke rezept online apotheke deutschland
farmacia online madrid: farmacias online seguras en españa – farmacia online españa envÃo internacional
farmacie online autorizzate elenco: acquisto farmaci con ricetta – farmacia online senza ricetta
farmacia online madrid: farmacias online seguras en espa?±a – farmacia online barata y fiable
vente de m?©dicament en ligne Pharmacie Internationale en ligne Pharmacie en ligne livraison Europe
Achat m̩dicament en ligne fiable: acheter m̩dicament en ligne sans ordonnance Рpharmacies en ligne certifi̩es
Farmacia online miglior prezzo: farmaci senza ricetta elenco – farmacie online affidabili
medikamente rezeptfrei: internet apotheke – europa apotheke
https://eumedicamentenligne.com/# vente de m?©dicament en ligne
Pharmacie en ligne livraison Europe Pharmacie en ligne livraison Europe pharmacie en ligne pas cher
apotheke online: shop apotheke gutschein – online apotheke preisvergleich
Farmacie online sicure: farmaci senza ricetta elenco – acquistare farmaci senza ricetta
internet apotheke: online apotheke – ohne rezept apotheke
Farmacie on line spedizione gratuita comprare farmaci online con ricetta farmacie online affidabili
medikamente rezeptfrei: shop apotheke gutschein – apotheke online
farmacia online 24 horas: farmacia barata – farmacia barata
internet apotheke: apotheke online – günstige online apotheke
pharmacie en ligne avec ordonnance: Levitra pharmacie en ligne – vente de m?©dicament en ligne
Pharmacie sans ordonnance: pharmacie en ligne – ?»?pharmacie en ligne france
Achat m?©dicament en ligne fiable: pharmacie en ligne sans ordonnance – pharmacie en ligne france fiable
pharmacie en ligne: kamagra oral jelly – Pharmacie sans ordonnance
pharmacie en ligne pas cher: cialis generique – trouver un m?©dicament en pharmacie
Viagra pas cher livraison rapide france Viagra sans ordonnance 24h Viagra en france livraison rapide
pharmacie en ligne fiable: kamagra oral jelly – Pharmacie Internationale en ligne
pharmacie en ligne fiable: cialis sans ordonnance – pharmacie en ligne
Pharmacie sans ordonnance: cialis generique – pharmacie en ligne fiable
Viagra homme prix en pharmacie sans ordonnance: Viagra generique en pharmacie – Acheter viagra en ligne livraison 24h
Hello!
This post was created with XRumer 23 StrongAI.
Good luck 🙂
pharmacie en ligne france livraison belgique: cialis generique – Achat m?©dicament en ligne fiable
pharmacie en ligne livraison europe: cialis generique – Achat m?©dicament en ligne fiable
https://kamagraenligne.shop/# pharmacies en ligne certifiées
pharmacie en ligne sans ordonnance: Levitra acheter – pharmacie en ligne france fiable
Viagra Pfizer sans ordonnance: Meilleur Viagra sans ordonnance 24h – Viagra homme sans ordonnance belgique
Hello.
This post was created with XRumer 23 StrongAI.
Good luck 🙂
My brother suggested I may like this blog. He was entirely right.
This publish actually made my day. You can not believe just how so much time I had spent for this information! Thank you!
My blog … eharmony special coupon code
trouver un m?©dicament en pharmacie: pharmacie en ligne france livraison belgique – pharmacie en ligne avec ordonnance
Pharmacie en ligne livraison Europe: Levitra pharmacie en ligne – pharmacie en ligne avec ordonnance
Viagra en france livraison rapide: Viagra homme prix en pharmacie sans ordonnance – Viagra g?©n?©rique sans ordonnance en pharmacie
Viagra femme ou trouver: Viagra g?©n?©rique sans ordonnance en pharmacie – Acheter viagra en ligne livraison 24h
pharmacie en ligne: pharmacie en ligne sans ordonnance – pharmacies en ligne certifi?©es
?»?pharmacie en ligne france: cialis prix – pharmacies en ligne certifi?©es
pharmacie en ligne france livraison belgique: Levitra 20mg prix en pharmacie – pharmacie en ligne france fiable
pharmacie en ligne france pas cher: pharmacie en ligne – Pharmacie sans ordonnance
trouver un m?©dicament en pharmacie: kamagra gel – acheter m?©dicament en ligne sans ordonnance
pharmacie en ligne fiable: acheter kamagra site fiable – pharmacie en ligne france livraison internationale
pharmacie en ligne fiable: levitra generique – pharmacie en ligne livraison europe
pharmacie en ligne france livraison belgique: achat kamagra – pharmacie en ligne france pas cher
Pharmacie Internationale en ligne: kamagra pas cher – Pharmacie sans ordonnance
pharmacie en ligne france livraison internationale: Acheter Cialis – pharmacie en ligne sans ordonnance
pharmacie en ligne france fiable: Pharmacies en ligne certifiees – Pharmacie Internationale en ligne
pharmacie en ligne sans ordonnance: Medicaments en ligne livres en 24h – pharmacies en ligne certifi?©es
https://levitraenligne.com/# pharmacie en ligne pas cher
Achat m?©dicament en ligne fiable: Levitra 20mg prix en pharmacie – vente de m?©dicament en ligne
Pharmacie Internationale en ligne: achat kamagra – pharmacie en ligne livraison europe
Pharmacie en ligne livraison Europe: kamagra 100mg prix – trouver un m?©dicament en pharmacie
Pharmacie sans ordonnance: cialis prix – pharmacie en ligne france fiable
pharmacies en ligne certifi?©es: Levitra acheter – pharmacie en ligne fiable
pharmacie en ligne sans ordonnance: Levitra acheter – pharmacies en ligne certifi?©es
https://autolux-azerbaijan.com/# Pin up 306 casino
Pin-up Giris: Pin Up Azerbaycan ?Onlayn Kazino – pin-up kazino
Pin-up Giris: pin-up360 – Pin-Up Casino
https://autolux-azerbaijan.com/# pin-up 141 casino
pin-up: pin up 360 – pin up onlayn kazino
pin up azerbaycan https://azerbaijancuisine.com/# pin up apk yukle
pin up onlayn kazino
medicine in mexico pharmacies: mexican pharmacy northern doctors – buying from online mexican pharmacy
https://northern-doctors.org/# medication from mexico pharmacy
buying prescription drugs in mexico reputable mexican pharmacies online reputable mexican pharmacies online
mexican pharmaceuticals online: mexican pharmacy – purple pharmacy mexico price list
http://northern-doctors.org/# mexico pharmacies prescription drugs
medication from mexico pharmacy: Mexico pharmacy that ship to usa – mexico drug stores pharmacies
buying prescription drugs in mexico: mexican pharmacy – purple pharmacy mexico price list
purple pharmacy mexico price list: buying prescription drugs in mexico – mexican online pharmacies prescription drugs
mexican online pharmacies prescription drugs: mexican pharmacy northern doctors – medicine in mexico pharmacies
https://northern-doctors.org/# mexico pharmacy
http://northern-doctors.org/# ?»?best mexican online pharmacies
mexican pharmaceuticals online: mexican pharmacy northern doctors – mexican pharmacy
mexican pharmacy: mexican pharmacy online – ?»?best mexican online pharmacies
https://northern-doctors.org/# mexican mail order pharmacies
https://cmqpharma.com/# mexico pharmacy
mexico pharmacy
reputable mexican pharmacies online online mexican pharmacy buying prescription drugs in mexico
best online pharmacies in mexico mexican pharmacy online buying prescription drugs in mexico online
mexican drugstore online
http://cmqpharma.com/# mexican drugstore online
buying from online mexican pharmacy
buying prescription drugs in mexico mexican pharmacy online mexican mail order pharmacies
mexican rx online cmq pharma mexican pharmacy mexican rx online
http://cmqpharma.com/# mexican pharmaceuticals online
medication from mexico pharmacy
http://indiapharmast.com/# top 10 online pharmacy in india
india pharmacy mail order: mail order pharmacy india – indian pharmacy paypal
buying prescription drugs in mexico online: mexico pharmacy – mexico drug stores pharmacies
mexican drugstore online: buying prescription drugs in mexico online – medicine in mexico pharmacies
legitimate canadian online pharmacies canadian pharmacy no scripts online canadian pharmacy
http://doxycyclinedelivery.pro/# doxycycline 20
ciprofloxacin 500mg buy online [url=http://ciprodelivery.pro/#]buy cipro online canada[/url] ciprofloxacin generic
https://doxycyclinedelivery.pro/# doxycycline tab india
http://paxloviddelivery.pro/# paxlovid india
how to buy cheap clomid [url=https://clomiddelivery.pro/#]get clomid online[/url] can you buy generic clomid
On March 31, 2010, the first manufacturing unit-built example rolled off the meeting line on the Detroit Hamtramck Assembly Plant, which served as a test for the
production line and high quality control functions, evaluating both tooling and pre-production automobiles before collection production commenced.
By October 2009, eighty pre-manufacturing Volts
had been constructed and subjected to testing below varied conditions.